It’s safe to say that most of us have experienced a scenario where we overreacted. Where we perhaps responded in a much more exaggerated fashion than the situation called for. Well, the same thing can happen to your cells in a condition known as mast cell activation syndrome – your mast cells can have a dramatic, overblown response and wreak havoc on your body from head to toe.
In recent years, our understanding of this complex condition has grown significantly. And as our understanding has evolved, so have our guidelines for diagnosis and our ability to treat these melodramatic mast cells.
Today we’re going to explore exactly what mast cell activation syndrome is, how diagnostic criteria have changed in recent years, and explore 2 fascinating new treatment strategies. Let’s dive in.
What Causes Mast Cell Activation Syndrome (MCAS)?
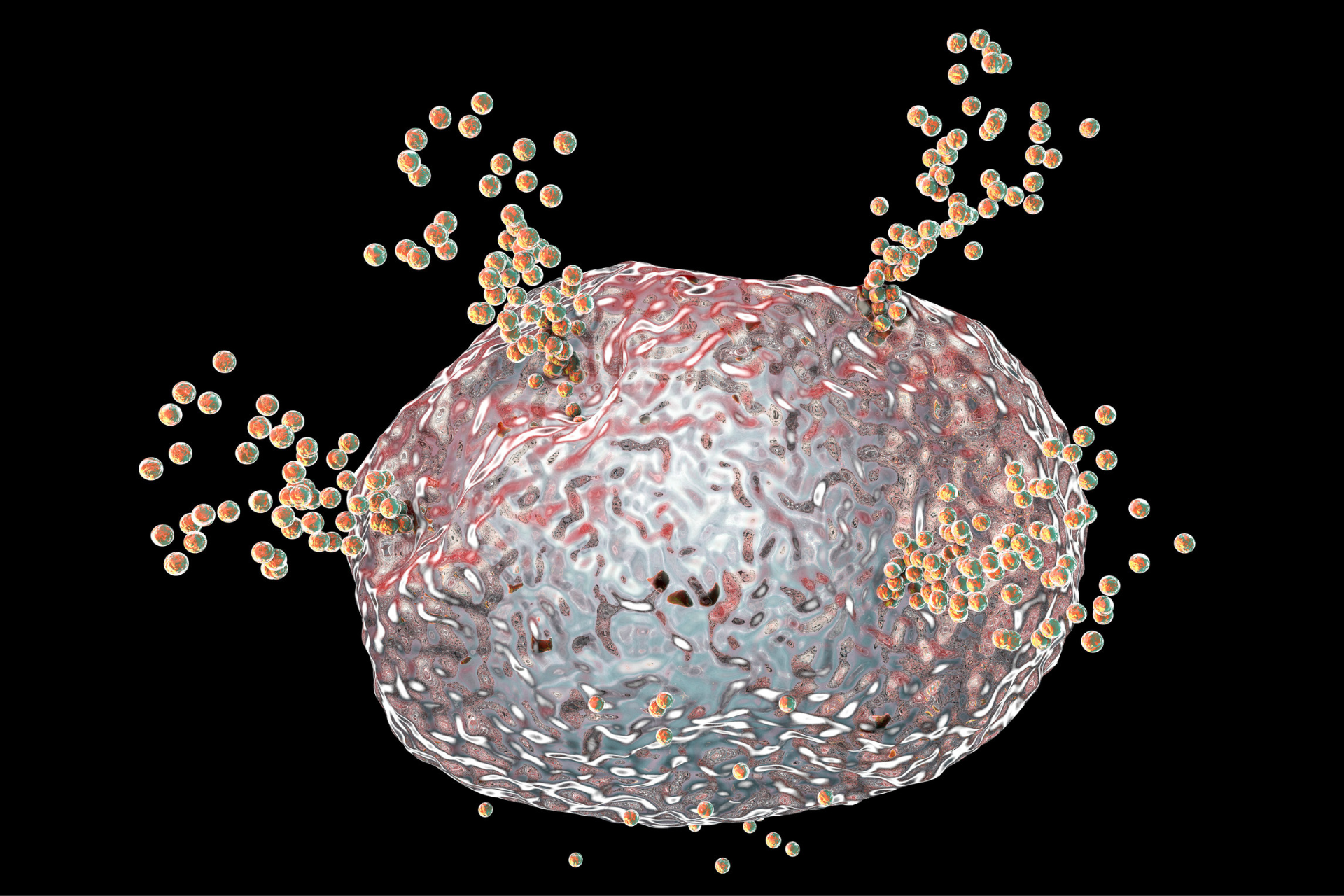
Mast cell activation syndrome, or MCAS, is a disorder caused by an over-reactive response from a group of cells known as mast cells. Mast cells are specialized immune cells that serve as a sort of alarm system. When mast cells detect a foreign invader they release a cascade of pro-inflammatory signaling molecules in a process known as degranulation.
When mast cells degranulate, they discharge these inflammation-stoking signaling molecules and activate your immune system. Normally, these mast cells degranulate, an inflammatory response is activated, the threat is neutralized, and then your body down-regulates inflammation to return to homeostasis.
But in MCAS, your mast cells begin to malfunction. They begin releasing far too many pro-inflammatory mediators far too often – creating a massive and sustained spike in inflammation. These misbehaving mast cells can create a host of tricky and distressing symptoms.1
What Are Symptoms of Mast Cell Activation Syndrome (MCAS)?
At a cellular level, the inflammatory response triggers:2,3,4
- The activation and recruitment of other immune cells to target and eliminate the invader
- Increased permeability of your tissues to more readily allow migration of immune cells
- Stimulation of bronchial and smooth muscle contraction
This combination of effects can induce a wide variety of symptoms that can impact every body system from head to toe. Just a handful of the symptoms MCAS can cause include:
- Flushing, hives, itching, swelling
- Digestive upset, nausea, vomiting, diarrhea, abdominal cramping, bloating
- A drop in blood pressure, rapid pulse, passing out
- Coughing, wheezing, shortness of breath, increased mucus production
- Brain fog, anxiety, headaches, difficulty concentrating, sleeplessness, vertigo
To get a much more in-depth look at the symptoms and bigger-picture diseases that can be triggered by MCAS, head over and read through my article Mast Cell Activation Syndrome: Here’s What You Need to Know When Histamine Goes Haywire.
How Do You Get Diagnosed With Mast Cell Activation Syndrome (MCAS)?
Diagnosing MCAS can be tricky because symptoms often include a vague and broad constellation of varying symptoms. As our understanding of mast cell activation syndrome has grown in recent years, there have been some adjustments to the criteria used to diagnose this disorder.
While these changes may seem slight at first, they can go a long way in enhancing our ability to accurately diagnose those suffering from the distressing effects that come with MCAS. Let’s take a little deeper look at the original diagnostic guidelines and how they've changed.
MCAS Diagnosis Consensus-1
The original guidelines for diagnosing MCAS are referred to as consensus-1 and encompass the following:5
- Typical clinical symptoms: Typical clinical symptoms are outlined as:
- Flushing
- Pruritus
- Urticaria
- Angioedema
- Nasal congestion
- Nasal pruritus
- Wheezing
- Throat swelling
- Headache
- Hypotension
- Diarrhea
- Increase in biomarkers: In consensus-1, the primary biomarker used for diagnosis is serum total tryptase. Any increase by at least 20% above baseline plus 2 ng/ml during or within 4 hours after a symptomatic period is required for a diagnosis of MCAS.
- Symptom improvement: A measurable response and improvement of symptoms when administered H1/H2 histamine receptor blockers or “mast cell-targeting” agents such as cromolyn.
According to consensus-1 guidelines, all three criteria must be met for an official MCAS diagnosis to be made.
MCAS Diagnosis Consensus-2
The updated version of diagnostic criteria has been dubbed consensus-2 and includes the following guidelines for MCAS diagnosis:5
- Typical clinical signs: Consensus-2 has a slightly altered description of clinical signs to include the presence of severe, recurrent episodes of systemic mast cell activation. Systemic is defined as including a minimum of two distinct organ systems and may include:
- Urticaria
- Flushing
- Pruritus
- Angioedema
- Nasal congestion
- Nasal pruritus
- Wheezing
- Throat swelling
- Hoarseness
- Headache
- Hypotensive syncope
- Tachycardia
- Abdominal cramping
- Diarrhea
- Biochemical markers: Consensus-2 also includes a 20% plus 2 ng/ml increase in serum tryptase level from the individual’s baseline, but extends to additional biochemical markers as well. Additional mast cell-derived biochemical markers that can be used for diagnosis include:
- Histamine
- Histamine metabolites
- PGD2 metabolites
- Heparin
- Symptom improvement: Consensus-2 also includes a measurable response and improvement of symptoms when administered the following drug therapies:
- Mast cell-stabilizing agents
- Drugs directed against mast cell mediator production
- Drugs blocking mediator release or effects of mast cell-derived mediators
Having broader and more robust diagnostic guidelines as seen in the updated consensus-2 criteria allows us to more accurately diagnose patients. And with increased diagnostic capabilities, we can better address symptoms and get patients on a path to management and healing.
What Is the Treatment for Mast Cell Activation Syndrome (MCAS)?
Treating mast cell activation requires a big picture approach and includes steps such as:
- Avoiding triggers
- Following a low histamine diet
- Taking mast-cell stabilizing drugs
- Taking low-dose naltrexone.
I’ve written extensively about some ways to address MCAS in the following articles:
- The Surprising Link Between Ehlers-Danlos Syndrome and Mast Cell Activation Syndrome
- 9 Proven Treatments for Mast Cell Activation Syndrome – Plus a Surprising Newcomer
- Mast Cell Activation Syndrome: Here’s What You Need to Know When Histamine Goes Haywire.
But there are a couple of additional treatment strategies that are proving to be heavy-hitters when it comes to treating MCAS.
How Else Can I Treat MCAS?
Two other, lesser-known underlying issues that need to be addressed when it comes to the treatment of mast cell activation syndrome include:
Addressing Trauma and Nervous System Dysregulation
Your mast cells, your vagus nerve (aka polyvagal system), and your limbic system work on an axis as part of your defense system. You see, there are mast cells essentially standing guard at each of your nerve endings. This creates a continuous feedback loop between your mast cells and your neurotransmitters – meaning your emotional state directly communicates and influences your mast cells.
This complex interplay means your nervous system, your emotional state, your stress levels, and your recurrent thoughts can have a monumental impact on your immune system and mast cell degranulation. Suppose your nervous system is dysregulated and consistently communicates to your mast cells that you’re in a stressed or unsafe state. In that case, your mast cells will go into a state of alert – heightening their sensitivity and increasing their likelihood of degranulation.
So an important component of treating MCAS is soothing these mast cells and helping them return to a balanced state. And one of the most crucial aspects of calming these mast cells is addressing nervous system dysregulation and any compounded trauma.
Addressing Mold Exposure and Underlying Infections
Your immune system has a complicated and delicate job. If your immune system is overwhelmed and overburdened, it can cause your mast cells to go haywire and begin over-reacting even to the slightest triggers.
So an important aspect of treating the dysfunction seen in MCAS includes addressing any underlying factors that might be contributing to your immune system burn-out such as:
- Mold exposure: You can read all about the link between mold and MCAS in my article Mold is a Major Trigger of Mast Activation Cell Syndrome
- Underlying infections: Hidden infections like Lyme disease, Babesia, Bartonella, or Eppstein Barr can put your mast cells into hyper-drive and contribute to MCAS.
- Toxin overload: If your exposure to environmental toxins exceeds your body’s ability to detox, these toxins can accumulate and damage your immune system. You can learn more about how toxin overload can put a damper on your immune system in my article How to Boost Your Immune System by Reducing Your Toxic Burden.
Eliminating underlying infections and supporting your body in detoxing from accumulated toxins is a key aspect of MCAS treatment.
Are you concerned about Mast Cell Activation Syndrome?
Mast cell activation syndrome is a serious and growing concern. Addressing this complex condition truly requires an entirely holistic and personalized approach to healing. But the good news is, if you're concerned about MCAS, you’re not alone.
There is hope and there is help. To learn more about MCAS and how you can take the first step in the journey to healing, start by reading through the articles linked above. And then I encourage you to head over and watch my interviews with the incredible Beth O’Hara where we talk all about the underlying causes of MCAS and the secret to addressing it. You can access them through the following links:
Knowledge is power. And with the right tools, you can heal from MCAS. If you enjoyed this article and want to take it to the next level, I encourage you to also sign up for my weekly newsletter by entering your name and email address in the form below. You’ll get my very best tips and resources delivered directly to your inbox.
Now it’s time to hear from you. Were you surprised to learn about some of the often-overlooked aspects when it comes to healing MCAS? Do you have any tips or inspirational stories about your journey to overcoming MCAS? Leave your questions or thoughts in the comments below!
Resources:
- Mast Cell Activation Syndrome: A Primer for the Gastroenterologist – PubMed (nih.gov)
- Mast Cell Activation Syndrome: Proposed Diagnostic Criteria – PMC (nih.gov)
- Characterization of Mast Cell Activation Syndrome – PMC (nih.gov)
- Mast Cell Activation Syndrome (MCAS) (aaaai.org)
- Diagnosis of mast cell activation syndrome: a global “consensus-2” (degruyter.com)
* These statements have not been evaluated by the Food and Drug Administration. The product mentioned in this article are not intended to diagnose, treat, cure, or prevent any disease. The information in this article is not intended to replace any recommendations or relationship with your physician. Please review references sited at end of article for scientific support of any claims made.


















13 Comments
This article is very interesting. I am being treated with antibiotics for chronic Lyme and Bartonella. I have very high Eosinophil count and have seen many drs.
The hematologist said when I asked about MCAS, that high eos was like mcas in my blood. Would the above referenced treatments help my health issue? Any other avenues I should try?
yes, possibly. High eosinophils may be related to MCAS. You might try some basic antihistamines like quercetin first
Please recognize the impact of sleep in managing MCAS. Sleep medications are less effective than behavioral sleep coaching due to the effects of poly pharmacy and the potential reactions to fillers. Patients who optimize their sleep will decrease over-activation of their autonomic nervous system and improve the functioning of their other organ systems.
I am an occupational therapist and a certified sleep coach w/hEDS and MCAS.
I would be interested in having you do an article on Hereditary Alpha Tryptasemia.
I have recently been diagnosed with it and now realize this has been a contributing factor in the severe food sensitivity problem I have had. I am struggling to find something that will help me since i am so sensitive to everything that I can’t tolerate and medications of supplement.
I took DAO with meals, all the supplements mentioned, and recently increased Loratadine to 3/day, added pepsid and other antihistamine at bed to help with 8 mo diarrhea since eating hidden food item (gluten, canola oil, corn, glyphosphate?)on flt to HA.
Dr says I have collagenous colitis and need steroid. Today only 4 diarrheas in am (vs 10 to 15 a day in afternoon and evening) Maybe Dr Kelly McCann is right. some need more. I also tried many other things that did not work.
Good Afternoon,
In the learning phase…very confused! Diagnosed with MCAS. Triptase level is a 17.3. None of my doctors have experience with MCAS. I am on Famotidine 20 mg & Loratadine 10 mg. I have been told to start immunotherapy. Contacted Dr. Afrin & Dr. Dempsey office in New York, appointments are two years out. Looking for help, need to find someone with experience in AZ or a surrounding state.
Question…
With a high Triptase level is it safe to do immunotherapy? Is it necessary?
Are my prescriptions(meds) appropriate until I can find a MCAS physician?
Thank you in advance for your time!!!
Hi Denise,
Best to talk to your immunologist on immunotherapy but all that you are doing sounds appropriate.
warmly
Dr Jill
Thank you for this very informative article! I have been suffering from MCAS due to surgical clips in my neck from hemithyroidectomy and gallbladder removal in 2005. My reaction was triggered by mononucleosis in 2015 leading to a type iv metal hypersensitivity. My case report can be found at the following link. Patients should be informed of medical device implants to avoid these type reactions because most doctors fail to be educated on the topic. I had to become my own investigator, researcher, and advocate or the systemic reaction would have lead to death. My surgical clip problems Facebook group saved my life! Members there have had to resort to teaching one another about these reactions and network to find doctors willing to remove the offending device. Please keep your readers informed on biological implant risk causing MCAS. We are most grateful for your work, thank you! https://www.cureus.com/articles/136554-diagnosis-and-management-of-a-hypersensitivity-reaction-to-titanium-containing-surgical-clips-a-case-report?fbclid=IwAR3ni1cGfKRs19lNjT2sOOYYloCjgV7JvZ0oY40mSBQa90DNgLk1NY-fOLE#!/
Thanks you so much for your coverage on Mast Cell Activation Syndrome McAS. Your coverage on this topic, like all your other articles over the years are very interesting and have led me on a different health track over the past several years. I now also go to a Naturopath MD, Functional Medicine doctor in Scottsdale. I will be sharing this with her since she has been working with me to lower my CRP and Homocysteine numbers, which are improving. I guess in reading the articles and links above, is it possible MCAS can lead to higher CRP? I do have poor sleep from elevated stress so we are working on stress reduction also in which my sleep is improving, now up to 5 hours of deeper sleep. My CRap was 10.3 a year ago and is now at 3, with a goal of under 1. I have changed my diet, and take a couple supplements that maybe are helping. THANKS again for all of your detailed articles. It was an article about 5 years ago, covering the 20 important blood tests that determine your overall health that led me away from traditional medicine to naturopath and functional medicine. Keep up the great work!!
Such an interesting article, from someone who seems to truly understand this debilitating illness. Thank you!
I have HEDS, Sjogrens & MCAS. I was given antihistamines & ketotifen to stabilise my mast cells, but sadly cannot tolerate them as they severely increase the dryness of my eyes (which is already severe). Are there any treatments you can recommend for MCAS that are not drying to the mucous membranes? My consultants just say I’m stuck between a rock & a hard place. I’m trialling DAO before meals currently & follow a low histamine diet.
Also, can I ask what drugs / supplements you would recommend for mould detoxification? I’ve been out of the mouldy water damaged property for 9 months, but symptoms continue. Hope to hear from you!
Kindest Regards Claire Brown
Thank you kindly, Claire!
Your question is a significant issue for many people. I would do low histamine diet and also try DAO with meals or cromomlyn. MCAS can take awhile to calm down but will eventually improve with detoxification.
warmly
Dr Jill
Hi Jill I am in Ontario Canada my 4 year old daughter has been suffering for two years and I honestly am worse than a low histamine low fodmap diet combined with her.
Is there a specialist in Canada or a resource that you could share that would be available in USA for us to use to our advantage, to guide us. We/she has dybiosis and I haven’t found out anything other than dybiosis, since she almost died at two and had far too many antibiotics to stay alive.
From a desperate mother alone in this battle.
Any response would be angelic and appreciated.
I need a doctor/guide to save her soul.
Hi Jenna,
I am sorry to hear it. You might try Dr. Lawence Afrin or Dr. Theo Theoharides.
warmly
Dr Jill
Share: