If you’ve ever experienced a runny nose, sneezing, or watery eyes, then you’ve experienced an allergic reaction. Allergens are bombarding our bodies all the time, and this reaction is a highly protective response by your immune system when mast cells sound the alarm.
Mast cells, also known as “jack of all trades” immune cells, are intricately involved in your body’s allergic response.1 They’re your first line of defense against foreign substances entering your body, and their central role is to protect you. Without them, your body wouldn’t even be able to heal from a wound.2
Mast cells are best known for the role they play in allergic and anaphylactic response. But, studies are revealing that they also play a significant role in immune activation, the development of autoimmunity, and increased inflammation.3
Unfortunately, mast cell disorders and mast cell activation syndrome (MCAS), in particular, are on the rise these days. I believe it’s in part because of the constant barrage of environmental toxins, molds, and chemicals.
Let’s take a look at what exactly mast cell activation syndrome is, how it might be causing your mystery symptoms, and what you can do.
What is Mast Cell Activation Syndrome?
Mast cell activation syndrome is an immune disorder. It’s just one type of mast cell activation disease.
What sets MCAS apart from other mast cell activation diseases is that it isn’t caused by an abnormally large amount of mast cells, and it isn’t a result of pathogen infection. Instead, when you have MCAS, you have a normal amount of mast cells, but they’re overactive and malfunctioning.
When your body is exposed to what it thinks is a threat, these overactive mast cells start to go haywire and secrete massive amounts of chemical mediators stored in the cytoplasm of your cells—degranulation. What’s meant to be a positive, protective response from your mast cells instead triggers both local and systemic negative effects.
When chemical messengers are released into your body, they set off an alarm that triggers an immune system response. And when this response becomes chronic—the chemical messengers are set off too much, too often—the result is mast cell activation syndrome.4
Mast Cell Activation Syndrome and Chemical Mediators
Mast cells are located near the border of just about every tissue in your body because they’re your first line of defense.
Mast cells are especially concentrated in your:
- Skin
- Gastrointestinal tract
- Lungs
- Sinuses
- Nervous system
- Reproductive organs
Because of their close location just below the surface of your tissues, mast cells are readily available to defend against foreign invaders as soon as they enter your body.5
If your immune system is working as it’s designed, it’s able to fight off these foreign invaders effectively. We see problems arise when your immune system goes into a constant state of reaction to allergens. When this happens, your body becomes flooded with histamine and other chemical mediators released by mast cells in response to the allergen.
These mediators include:6
- Histamine
- Tryptase
- Chymase
- Interleukins
- Prostaglandins
- Cytokines
- Chemokine
- Proteases
These chemical mediators are responsible for affecting early phases of allergic reactions. And once these chemical messengers are released into your system, they can trigger even more late-phase and systemic effects.
When you have MCAS, you have repeated episodes of symptoms, although the organ systems that are affected and the combination of symptoms does vary. Let’s take a look at the variety of symptoms caused by overactive mast cells.
What Are the Symptoms of Overactive Mast Cells?
Symptoms associated with MCAS are caused by large amounts of histamine in your body when mast cells become hypersensitive and overactive. I’ve found that even with the huge variation of symptoms that can be present, the number one complaint from my patients with MCAS is often fatigue.
Along with chronic fatigue, here’s a list of symptoms I most commonly see in my practice that cause me to suspect mast cell activation in my patients:7,8,9,10
- Skin-related symptoms of overactive mast cells:
- Hives
- Itching
- Swelling
- Flushing
- Gastrointestinal-related symptoms of overactive mast cells:
- Nausea
- Vomiting
- Diarrhea
- Abdominal cramping
- Bloating
- Cardiovascular-related symptoms of overactive mast cells:
- Low blood pressure
- Rapid pulse
- Passing out
- Vascular permeability (inflammation and swelling)
- Respiratory-related symptoms of overactive mast cells:
- Wheezing
- Shortness of breath
- Cough
- Asthma-like symptoms
- Sinusitis
- Rhinitis
- Increased mucus production
- Brain-related symptoms of overactive mast cells:
- Brain fog
- Anxiety
- Headaches
- Difficulty concentrating
- Sleeplessness
- Neuropathic pain
- Vertigo
What Diseases are Associated with Mast Cell Activation Syndrome?
A growing body of research reveals that mast cells play a key role in the early stages of many diseases. The list I give below is likely not all-inclusive but includes some of the ones that have been identified so far as being associated with MCAS:11,12,13,14,15,16,17
- Allergies
- Asthma
- Atherosclerosis
- Autism
- Autoimmune diseases (Hashimoto’s thyroiditis, systemic lupus, multiple sclerosis, bullous pemphigoid, rheumatoid arthritis)
- Eczema
- Ehlers-Danlos syndrome
- Celiac disease
- Chronic fatigue syndrome
- Chronic inflammatory response syndrome
- Eosinophilic esophagitis
- Fibromyalgia
- Gastroesophageal reflux
- Infertility (mast cells in the endometrium may contribute to endometriosis)
- Interstitial cystitis
- Irritable bowel syndrome
- Migraine headaches
- Mood disorders: anxiety, depression, and insomnia
- Multiple chemical sensitivities
- Postural orthostatic tachycardia syndrome (POTS)
What Triggers Mast Cell Activation Syndrome?
Since 2007, when MCAS was officially recognized, our knowledge about the syndrome has increased significantly.18 But the reality is, even with this new data, we still have a lot of questions about MCAS.
One of them is: exactly what triggers the activation of mast cells and causes them to malfunction in the first place?
A severe flare-up of symptoms might be triggered by pollen in the spring, while a flare-up in the summer might be due to heat and increased exposure to sunlight. Unfortunately, we really can’t be sure exactly what the triggers are when it comes to MCAS. But, the good news is, even with these uncertainties, we do have a basic idea of potential triggers of mast cell activation. 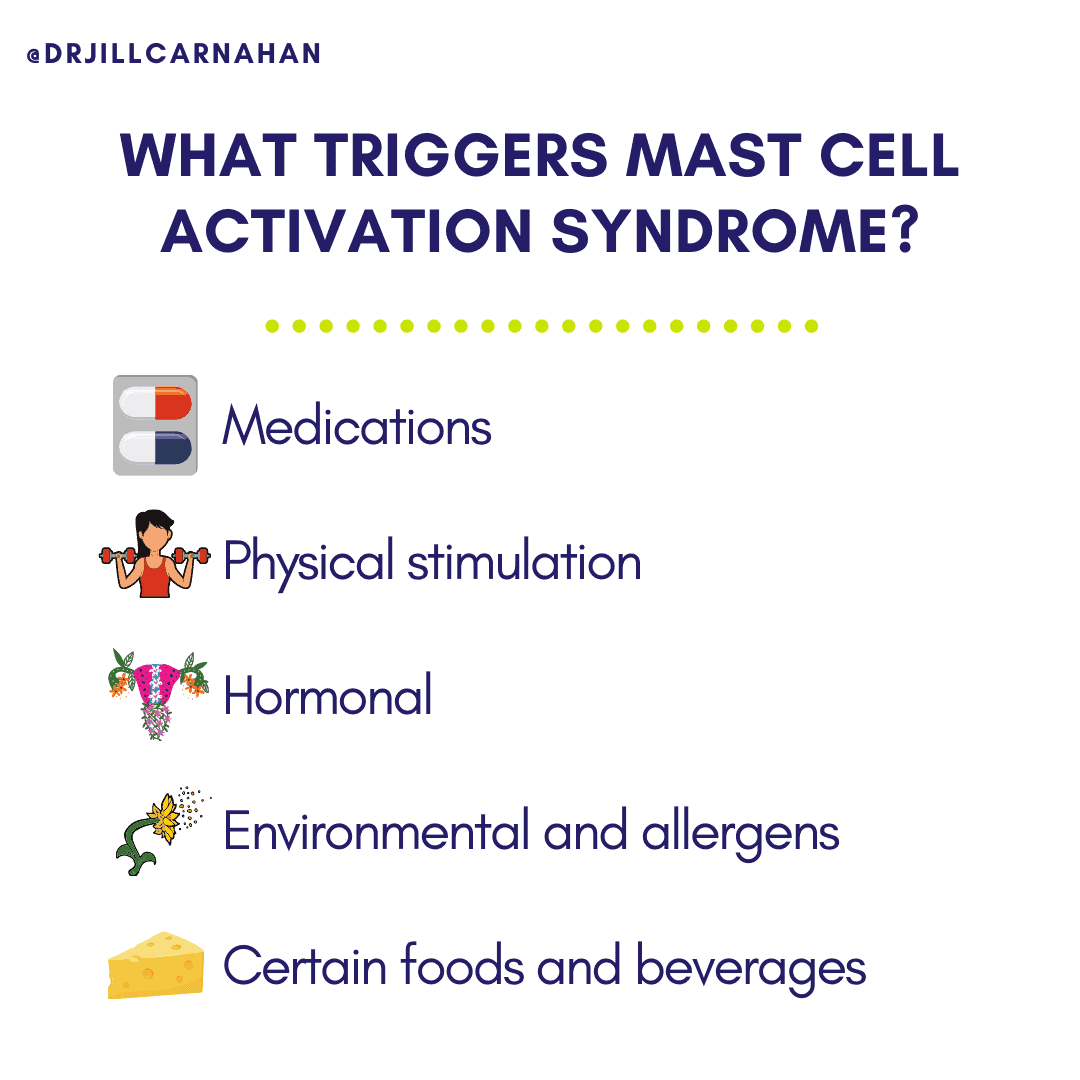
Let’s take a look at some of the triggers that can throw malfunctioning mast cells into overproduction mode:19,20
-
- Medications: narcotics, opioids, NSAIDs, muscle relaxers, supplements, antibiotics, anesthetics, contrast dyes
- Physical stimulation: heat, cold, pressure, pain, trauma, exercise, ultraviolet light, electrical stimuli, osmotic stimuli, friction and vibration, fatigue
- Hormonal: estrogen, progesterone, a-MSH, CRH, emotional stress
- Environmental and allergens: venoms, environmental antigens, pollen, perfumes, chemical odors, natural odors, pet dander, infections, pollution, mold
- Certain foods and beverages: foods and beverages high in histamine (more on this later)
We know that overactive mast cells play a significant role in exacerbating autoimmunity. But the triggers that can cause mast cells to become hypersensitive are vast, as you can see above, and highly variable.
How is Mast Cell Activation Syndrome Diagnosed?
Diagnosing MCAS is difficult in part because we still don’t have a consensus for objective guidelines for a diagnosis. Despite a lack of consensus, a diagnosis of MCAS is sometimes given when a wide variety of signs and symptoms are present without a known trigger and other possible diagnoses have been ruled out.
When a specific trigger can’t be identified and the mast cell activation doesn’t appear to have a known cause, it’s known as idiopathic.21
The first step I take with my patients is to determine if unexplainable symptoms like itching, flushing, gastrointestinal disturbances, systemic hypotension, and fluctuations in blood pressure are better explained by another diagnosis. The next step is to determine if these symptoms can be eliminated through routine treatment.
If symptoms aren’t eliminated, I’ll do a workup to see if there’s a known allergic basis for the symptoms. This allergic basis falls under two categories:
- Primary: activation of mast cells by mutations resulting in an abnormal amount of cells
- Secondary: external triggers like allergic antibodies or infection
If what’s going on doesn’t seem to fit in either the primary or secondary category, and if mast cells are found in a normal amount but are hyperresponsive, then I suspect mast cell activation syndrome.22
When I make a diagnosis of MCAS with my patients, I use this commonly accepted criteria. I look for two or more of the following:23
- Two or more organs that show symptoms of mast cell activation, such as wheezing, flushing, diarrhea, and hives.
- Two episodes with elevated levels of chemical mediators such as 11β-PGF2, serum tryptase, or 24-hour N-methylhistamine.
- At least one episode with serum tryptase consistently greater than 15 ng/ml.
- Primary and secondary disorders, such as systemic mastocytosis or a clonal mast cell disease, have been ruled out with a negative bone marrow and tissue biopsy.
Although not necessarily a criteria for diagnosis, I consider the improvement of symptoms with drugs that target mast cell mediators as more evidence pointing to MCAS.24
Currently, we only know of a few biomarkers that implicate mast cell activation as the root cause of various symptoms and diseases. More research is needed to help us make a more definitive and accurate diagnosis.25
How is Mast Cell Activation Syndrome Treated?
While mast cell activation syndrome isn’t curable, if you’ve been diagnosed with mast cell activation syndrome, you do have treatment options available to help you manage your symptoms.26
Because of the wide range of possible symptoms caused by mast cell activation syndrome, treatment will need to be tailored specifically to you and your symptoms. Thankfully, research studies on effective treatment options for sufferers of mast cell activation syndrome are ongoing.
Antihistamines are typically the first course of treatment I recommend because they target the overwhelming amount of histamine produced by mast cells. I highly recommend Hist Assist to my patients. It’s a very effective antihistamine with a targeted blend of all-natural ingredients that create a powerful combination to promote optimal health and provide you with relief from mast cell activation syndrome symptoms.
For a more comprehensive course of treatment, here are three basic options to help manage your symptoms.
Three Basic Treatment Options
We know that mast cell activation syndrome results from overactive mast cells. So, inhibiting and stabilizing them is an important step in managing your symptoms. There are three basic treatment options that are generally used:27,28,29
Inhibit the production of mediators through the use of:
- Steroids (short term use, ideally)
- Non-steroidal anti-inflammatory drugs
- Immunomodulatory drugs
Inhibit the release of mediators by stabilizing mast cells using:
- Benzodiazepines
- Cromolyn
- Pentosan
- Alpha interferon
- Tyrosine kinase inhibitors
- Ketotifen
- Omalizumab
- Quercetin
Block the release of mediators through:
- H1 and H2 receptor blockers
- Leukotriene antagonists
- Bisphosphonates
Beyond these basic therapy treatments, there are more options available that work by targeting specific symptoms caused by mast cell activation syndrome. For an in-depth look at more treatment options, I’ve listed several effective ones in my article 9 Proven Treatments for Mast Cell Activation Syndrome—Plus, a Surprising Newcomer.
I know that trying to figure out the best medications and supplements to treat your symptoms can be daunting. Not to mention, time-consuming. When you have a lot of options in front of you, it can be hard to know where to start and what’s best. To help reduce overwhelm, I recommend you take a look at your diet as an easy first step.
Becoming familiar with foods high in histamine, so you know what to avoid, is a natural place to start.
High-Histamine Foods to Avoid
Mast cell activation syndrome can make you highly reactive to a wide variety of food. 30 So, avoiding foods that are high in histamine can help you identify foods you’re sensitive to. You might find that you’re able to consume some of the foods restricted on a low-histamine diet and tolerate them well.
I suggest you use the following list as a general guideline and start by eliminating all of these foods in the beginning. Then, you can choose to add certain foods back into your diet. Always be sure to take note of how you feel when you’ve added a food back in, so you can recognize what, if any, symptoms reappear. Keeping a food journal is a great way to do this.
Here’s a list of the top high-histamine foods you’ll want to avoid:31
- Fermented dairy products, such as cheese, kefir, yogurt, buttermilk, and cream cheese
- Fermented vegetables, such as kimchi, sauerkraut, and pickled vegetables
- Fermented soy products and some legumes, such as soybeans, red beans, green peas, sugar snap peas, and sweet peas
- Some fruits, including all citrus, berry, and stone fruits, along with bananas, grapes, pineapples, and over-ripe fruits
- Some vegetables, including avocados, eggplant, spinach, white and sweet potatoes, tomatoes, and over-ripe vegetables
- All shellfish, canned fish, cured meats, and pickled meats, eggs, and fish
- Walnuts and pecans
- All processed oils with preservatives BHA and BHT
- Some herbs and spices, such as cinnamon, clove, anise, curry, cayenne, and nutmeg
- Processed sweeteners and sugar products, chocolate, cocoa, and unpasteurized honey
- Products made with yeast and yeast extracts
- Bleached flour
- All alcohol, teas, fruit drinks, carbonated drinks, and nonalcoholic beers and wines
- All vinegars, ketchup, and mustard (with vinegar), and relish
- All artificial preservatives and food dyes
If you decide to add any food back into your diet, my recommendation is to continue avoiding, or at the very least limiting, all processed foods, artificial preservatives and sweeteners, sugar, dairy, wheat, and restricted spices.
And, as an extra measure to help you control the amount of histamine you consume from food, I recommend Histamine Blocker to my patients. This patented supplement is formulated to help your body combat excessive histamine found in the food you eat.
Where Do You Go From Here?
Mast cell activation syndrome is complicated because it can have both common and unusual symptoms that affect you on a multisystemic level. A doctor who’s familiar with this lesser known syndrome will help take the mystery out of what’s going on in your body. And, the information in this article is an excellent way for you to get started on your path toward healing.
It’s important that you work with a doctor who’s familiar with mast cell activation syndrome and the various ways it shows up.
If you have or suspect you have mast cell activation syndrome, you might feel overwhelmed and uncertain about what you can do to lessen your symptoms and improve your health. Know that most sufferers of mast cell activation syndrome are able to find an effective strategy that works for them and helps them feel significantly better. But, it will take patience, persistence, and an approach that’s made specifically for you and your symptoms.
Now I want to hear from you. Do you suspect you have mast cell activation syndrome or have you already been diagnosed with mast cell activation syndrome? Have you found antihistamines like Hist Assist to be helpful in managing your symptoms? Let me know in the comments!
Has there ever been a time in your life when you’ve felt alone or unsure where to turn for answers?
In Unexpected: Finding Resilience through Functional Medicine, Science, and Faith, Dr. Jill Carnahan shares her story of facing life-altering illness, fighting for her health, and overcoming sickness using both science and faith so that others can learn to live their own transformative stories.
Dr. Jill’s riveting and compassionate exploration of healing through functional medicine demonstrates how to replace darkness and fear with hope and find profound healing, unconditional love, and unexpected miracles in the process.
Resources:
1 https://www.sciencedirect.com/science/article/pii/S0925443911000445
2 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4424662/
3 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3597223/
4 https://mastcellactivationsyndrome.org/
5 https://www.sciencedaily.com/releases/2010/06/100607111308.htm
6 https://www.sciencedirect.com/science/article/pii/S0925443911000445
7 https://www.jillcarnahan.com/downloads/MCAS-Afrin.pdf
8 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3753019/
9 https://www.aaaai.org/conditions-and-treatments/related-conditions/mcas
10 https://jhoonline.biomedcentral.com/articles/10.1186/1756-8722-4-10
11 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5341697/
12 https://www.nature.com/articles/s41598-019-38679-4
13 https://www.ncbi.nlm.nih.gov/pubmed/25941080
15 https://www.jillcarnahan.com/downloads/MCAS-Afrin.pdf
16 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4888802/
17 http://www.dysautonomiainternational.org/blog/wordpress/a-tale-of-two-syndromes-pots-and-mcas/
18 https://www.jillcarnahan.com/downloads/MCAS-Afrin.pdf
19 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3069946/
20 https://www.ncbi.nlm.nih.gov/pubmed/18680704
21 https://www.aaaai.org/conditions-and-treatments/related-conditions/mcas
22 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3753019/
23 https://www.ncbi.nlm.nih.gov/pubmed/17537151
24 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3753019/
25 https://www.jacionline.org/article/S0091-6749(18)30854-6/fulltext
26 https://www.jillcarnahan.com/downloads/MCASReview.pdf
27 https://www.jillcarnahan.com/downloads/MastCellActivationDxandTxMolderings.pdf
28 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4903110/
29 https://www.jillcarnahan.com/downloads/MCAS-Afrin.pdf
30 https://www.jillcarnahan.com/downloads/MCAS-Afrin.pdf
31 https://histamine-sensitivity.com/histamine_joneja.html
* These statements have not been evaluated by the Food and Drug Administration. The product mentioned in this article are not intended to diagnose, treat, cure, or prevent any disease. The information in this article is not intended to replace any recommendations or relationship with your physician. Please review references sited at end of article for scientific support of any claims made.


















248 Comments
Dr. Jill-
Your presentation at the CIRS Conference was amazing! You are such a dynamic Physician , educator and healer. I am on moldy house #4. I keep jumping out of the frying pan into the fire. I was treated with CSM 3 years ago when I was exposed to Chaetoneum. Initially, I would sweat profusely upon expose. Then I started having an immediate bowel movement when I was around something I didn’t like ( I have to laugh). Now, I have EMF sensitivity that is causing me to go into seizures. I just moved to a new area and am trying to find Integrative Health Care. Psychiatrists that understand the effects of mold are seemingly impossible to locate. I am a mercury poisoned Dental Hygienist with MarCons and a husband that doesn’t want to move again. I am extremely resilient but I am at the end of my rope. Do you do phone consults? I am the poster child for CIRS and MCAS….
Gratefully,
Kay Helfant
Hi Kay. The EMF issue is most often if not always a Mercury issue, Definitely avoid Smart Meters, Wifi as much as possible esp on Hand Held devices but even being around it at all, and cordless phones (an cells) are all especially bad. I hope you look to safe Chelation, the safest and most effective being the Andy Cutler Chelation Protocol, which unfortunately most Doctors are not using. Good healing to you, sorry you too are poisoned (I am as well as are many others I know personally).
Dear Kay,
I am sorry to hear of your suffering… you might try searching in your zip code for functional medicine trained physicians at http://www.ifm.org. I am not currently taking new patients but you may check back anytime
Warmly
Dr Jill
Thank you for shinning a light on this again. I have felt that Mast cells were the driver of my CIRS and chronic fatigue for about 3 years, and the driver of my interstitial cystitis for 7 years, but because of my very painful interstitial cystitis I can not tolerate any of the ingredients in Hist Assist or most other supplements and many herbs. Is there something more soothing for the bladder that would help in regard to the mast cells?
Do you recommend dehydrated organ meats like kidney which are high in DAO? Are dehydrated organ meats high in histamines as I understand aged meat is? I tolerate fresh meats very well.
Do you feel dehydrated organ meats are a net positive or negative for a situation such as mine?
Preserved, dried or jerky meats may have high histamine content
Hey kay! check out juice fasting with histamine tolerance mcas on YouTube, a woman speaks to this
Hello. My son had an illness 4 years ago that doctors never diagnosed however they speculated he had an undiagnosed case of encephalitis. Since then, he has experienced several ‘flare ups’ of a cognitive fog which eventually leads to insomnia , inability to find words, difficulty communicating and anxiety. He never had these issues prior to his illness four years ago. We cannot find common triggers for when the flare ups happen. His symptoms match many of those you have listed in this article. We’ve been to 18 doctors in all different disciplines given his wide range of symptoms. Wondering if there is a list of doctors who specialize in mast cell activation diagnosis that I can take him to? Thank you!
You might try the world expert, Dr. Lawernce Afrin….
Sounds like Lyme Disease.
lyme can be a trigger to MCAS
lyme can be a trigger to MCAS
Hello! Great read. For a long time I have had many medical issues, not severe, more of a chronic state of not well. I am in the process of being diagnosed with EDS, a previous doctor of mine thought I shouldnt peruse the diagnosis because treatment is mostly preventative but the longer I have gone sense that point the more I feel I need to find a name for the many little issues I have with my body. Recently I got information from an oral pathologist in regards to unexplainable lip swelling I have had and got pointed towards MCAS. In addition to possibly explaining my lips, from what I have been reading it seems like it also may explain throat/ eye swelling reactions I have as well and abdominal pain and vomiting. A long explanation for a simple question, is MCAS tied to geographic tongue in any way? It is another reaction I have almost constantly and I am just curious if it tied in. I feel like that more I learn the more I feel like all my little weird things are able to be attributed to a bigger issue.
hi have you found any relief? i have GT and gut problems and eating 5 foods for 2 years. react to all supps and meds. dont know what to do. im deteriorating
Dr. Jill – thank you for your informative article! It’s great to understand the mast cell activation syndrome. My chiropractor found my histamine problem through genetic testing/MethylGenetic Nutrition Analysis, and Professional Health Products Histamine Scavenger solved my problem (I previously had the IgG test to know what foods to avoid). My CFS is gone, my FMS is almost gone and I sleep well for the first time in decades. I love PHP products so much that I became their Colorado rep:)
Hi Angie,
thanks for sharing your story!
warmly
Dr Jill
Hi Jill
I am in France. Do you know of a similar product in Europe to a Histamine scavenger please.
Kindest regards
Janet
Hi Janet,
I believe UmbrellexDAO is from Europe
warmly
Dr Jill
Hi Jill, I’ve just read your article and I have to say it’s the best one that really puts everything out there in simple terms. I have no exact diagnosis but I suspect MCAS and HIT. I’ve been dealing with chronic symptoms for many years. Would you be able to suggest a product similar to Histamine Scavenger that I could get in Canada. Thanks so much for your knowledge!!!
Doctorts that treat mass cell in houston area
Hi John
You may not be able to find a local expert but I suggest Dr. Lawence Afrin or Dr. Theo Theoharides.
Hi Angie,
What foods did they suggest? I have it in my bladder and can’t figure it out. It’s getting worse. Thank you so much! Debbie
How can I order from you?
you can order online products here https://www.drjillhealth.com
Thank you so very much for this article . I was diagnosed with IBS, dispute having Adhesions removed from my Colon in 2015. Unlike the normal person who has IBS occasionally; I have pain every day. I would like to look into the Mass Cell Activation. I live Las Vegas;. Do you know of any doctors out here who do this?
Hi Jennie
You might try contacting world expert, Dr. Lawrence Afrin, to get a referral in your area
warmly
Dr Jill
Dr. Carnahan, I see you have a great article on Mast Cell Activation and a bit about Histamine Intolerance, for some great help for people that suffer from one or both of these, I would highly recommend http://healinghistamine.com This site has been very helpful to me and many I meet who don’t know much about histamine intolerance. Thanks for addressing this very challenging topic!
Dr Carnahan,
I am reading through the diet recommeded for MCAS by Dr Joneja in the link you give above and there are quite a few surprises on the list so can you comment? My wife follows a different list from Dr Ahern (in addition to strict Paleo) and it seems to help but the list in your link seems strange (why does it allow dairy, gluten and cashews for instance).
I am specifically interested in why the following are restricted:
Sweet potatoes
Berries such as blueberries, blackberries
Grapes
Unpasteurized honey
Thanks for your help!
Dr. Joneja’s diet eliminates foods that contain high histamine levels. The Paleo diet is not focused on histamine levels in food.
warmly
Dr Jill
I don’t know if I just simply have a salicylate and histamine intolerance or if its mast cell activation. I just know that I react to many vegetables , fruits, preservatives,dyes, yeast, fermented things etc. I have completely eliminated gluten products because I was getting brain fog so bad it felt like I got a concussion along with numbness and pins and needles. although putting aside the gluten from food I still get flushing , burning skin, and onset of extreme anxiety. The thing that confuses me if how fast the reaction will come on it will take often less than a minute to start having my skin burn and when I react wrong to a food and get anxiety it happens in less than a minute to and sometimes will last all day so I try to be so careful what I eat. I don’t understand what would be causing me to get such fast reactions from food. Its been hard.
That sounds like a histamine IgE reaction since it occurs very quickly. It could also be sensitivity to oxalates in food or salicylate. I suggest further testing to determine the cause.
warmly
Dr Jill
Dr Carnahan, I love your work. I’m a nutrition consultant that specializes in children with autism. I work a great deal with low salicylate and amine diets, as well as low oxalate. I know salicylates can trigger mast cells, but (based on your comment) can oxalate trigger mast cell activation? Or were you simply suspecting another (unrelated) type of reaction from oxalate?
I suspect that both of these chemicals and the dysbiosis driving them may trigger mast cell activation.
If one can assume it is longstanding dysbiosis causing MCAS, then could fixing the dysbiosis, and maintaining eubiosis allow the mast cells to calm down and one could be “cured”? Or is it once they become hyperactive they cannot return to normal functioning?
Hi John,
yes when dysbiosis contributes to excess histamine or MCAS symptoms, treating the gut issues will often resolve the symptoms
warmly
Dr Jill
Wow, this article is amazing. I suffered for many years with chemical sensitivities, asthma, allergies & digestive issues. For about 10 years I had even had seizures. Doctors said I had everything from Lymes disease to MS, but nothing was concrete. My husband & I operated a commercial cleaning business for 20yrs. Now he has a lot of the same problems as me. Doctors have been treating him for RADS, asthma & COPD. We found the only way to cope was to be guarded about our environment. We discontinued our business, which helped me to improve, but he continues to decline. Thank you for the research going into understanding this growing problem.
For a more natural approach what do you suggest in supplementations and eating to stabilize the mast cells rather then taking any medicine. Please advise and Thank you!
Hi Judy
I have listed all the natural mast cells stabilizers in article here
Warmly
Dr Jill
Thank you for this article Dr Gill. I saw 2 allergists here in quebec, canada, and have an appointment with a third one soon, since no one helped me, they only do the skin scratch tests to confirm i have pollens, dust, cats and seafoods ige mediated allergies. Now that doesnt help me at all with my mcas symptoms, i evrn had POTS symptoms last summer that fortunatly calmed down since my diet is very stable with testing every safe food separatly ( im eaTing about 30 different foods now). My question is: how do i make sure the allergist does me the good tests to diagnose possible mcas? I cannot travel far to see a specialist, i cannot eat out and im a single mother of two. I do not take any medication. Im afraid to go back to the dentist ( had a cardio respiratory reaction with anesthesiant) . My typical reaction is sensation that something is stuck in my throat. I have much itchiness and redness on the skin. Stomach pain. Thanks for helping me.
Mona, my wife’s story mirrors yours. From the something stuck in the throat, pins and needles, bad dental experience with elevated heart rate for weeks, Benadryl had opposite effect, rashes hives , Ibs, down to potatoes, green beans,eggs, carrots, Haagen Daz vanilla ice cream ONLY. Everything else pretty much causes problems… what foods sit well with you? I gotta get my wife above 95 lbs. thanx:)
Dear Dr. Jill
Do you have ever studied or considered the relation between the MCAS and periodic fever syndrome as PFAPA?
My son has allergies and now it seems he has PFAPA.
Dear Dr. Jill
Do you have ever studied or considered the relation between the MCAS and periodic fever syndrome as PFAPA?
My son has allergies and now it seems he has PFAPA.
It could be related but I have not seen any research on this…
I was not aware that MCAS is related to inflammation my son’s allergies are always related to food and he always had vomits and diarrhea and very specific times rashes. I believe he had FPEIS to rice. We have controlled the trigger foods (no diarrhea or vomits anymore) but he’s still bloated and underweight but growing. One year ago he started with fevers that follow a pattern we are about to get a Periodic fever syndrome diagnosis.
I really wonder if MCAS and PFAPA could be connected and maybe using some of the natural tratement that you mentioned could help.
Btw PFAPA is controled with corticosteroids
ALA is a powerful Mercury chelator and crosses the blood brain barrier. It should only be dosed low, slow and frequently based on its half-life–and only if there are no Mercury fillings in the mouth. Otherwise, one risks redistribution of the Mercury throughout the brain and body.
Hi HC
Yes, ALA must be used with caution but most patients can tolerate low dose R Lipoic Acid
warmly
Dr Jill
Just because Andy Cutler says that doesn’t make it so. That hypothesis has been proven to be inaccurate.
Hi Dr. Jill,
I have been trying claritin once a day in the morning or Benadryl once in the evening (rather than the claritin) and I am noticing a MAJOR decrease in my night-time pain attacks due to my Crohn’s disease. Since starting the histamine blockers listed above I have been able to stop taking nightly narcotics for the pain. I am also on Stelara so I need to figure out which is causing the breakthrough but the reason I tried this is because I was continuing to have pain despite the stelara. This could be a MAJOR breakthrough for me. I am going to do some experiments where I go off the histamine blockers for a week and see what happens, though I am reluctant to mess with a good thing. Very exciting.
Eve
Wonderful, Eve! I hope this continues to help you…
Dr. Carnahan,
How does one get a diagnosis of MCAS? What specialist is likely to do the diagnosing or order more tests? Immunologist, allergist, dermatologist? My PCP isn’t very open or helpful in discussing other possibilities of all of my vague symptoms. I have always had extreme/severe allergies that cause respiratory symptoms. I am very sensitive in general, to medications and environmental. I have seen an allergist off and on for about 15 years so I do have confirmed allergies. Lately I have “unknown” allergens when I eat and cause nose stuffiness and some facial tingling but no answers as to what is causing it…just that I now need to carry an epi-pen with me. I have a chronic history of: joint swelling/inflammation/stiffness mainly in my hands and back, chronic headaches and 2-3 migraines a month, I bruise extremely easy, insomnia, i flush easily and get hives on my forearms, chronic vit D deficiency, osteopenia, and bone infections in the jaw (4 rounds of antibiotics for that). Starting in 2015 I noticed heart palpitations intermittently after I started antibiotics. they still come and go. Around the same time I started having low blood pressure and have had a few instances of passing out. I was told by my PCP it’s probably just dehydration and to drink plenty of fluids. It’s frustrating to try to piece it all together and get answers. I don’t want to mask symptoms any longer.
MCAS is a clinical diagnosis. Symptoms consistent with MCAS and response to treatment.
warmly
Dr Jill
Hi Dr. Jill,
I am wondering if you have come across joint hypermobility and Ehlers-Danlos syndrome in relation to mast cell disorders? Thought you might want to add it to your list of associated conditions.
This article was just recently published. http://onlinelibrary.wiley.com/doi/10.1002/ajmg.c.31555/full
Thank you for all your great articles!
Chris
I concur with this comment. I stumbled across this article and was surprised to not see EDS listed.
because EDS is a known to be co-morbid with mast cell problems
Love your article & it was recommended by my Rheumatologist. I’m labeled with lots of conditions, Unspecified IBD/IBS, Inflammatory Autoimmune Disorder, Chronic Migraines, CFS, Fibromyalgia & a mental case! Recently diagnoised with Autoimmune Urticaria due to positive Basophilic Activation & a Mast Cell Disorder with extremely high IgE Fc Receptor AB & symptoms. Whatever the label is, it attacks my Skin, GI, Brain, Heart (Electrical) & my joints. I have 2 questions.
1. Can this disorder cause lesions in the white matter of the brain on MRI?
2. Best approach in discussing Mast Cell Disorder with a doctor who is unfamiliar or doesn’t believe the condition exsists?
Thank you for you time & education in these matters!
Hi Lynn,
I do not think MCAS can cause white matter lesions in the brain. Best approach would be to share the resources from Dr. Theoharides and Dr. Afrin
Warmly
Dr Jill
any condition that involves untreated (or under-treated) chronic pain *WILL* cause damage to the white matter of the pre-frontal cortex, resulting in concentration problems and issues with working memory transfer. This is just one of many serious health problems caused by not treating pain.
any condition that involves untreated (or under-treated) chronic pain *WILL* cause damage to the white matter of the pre-frontal cortex, resulting in concentration problems and issues with working memory transfer. This is just one of many serious health problems caused by not treating pain.
I would say to really consider Lyme disease and co-infections, such as Bartonella, Babesiosis, etc. Lyme disease and its co-infections can cause all of those symptoms, including activate ‘autoimmune disorders’ in susceptible people. Possibly find a good Lyme Literate Medical Doctor (LLMD) or a Lyme Literate Naturopathic Doctor (LLND). Unfortunately, the testing for these pathogens is poor, especially the tests from Quest and Labcorp. A good LLMD or LLND will use other labs, such as iGeneX labs, Galaxy labs, etc. There are other tests too, such as CD75 NK Cells test that seems to be better than most tests to help determine chronic Lyme disease, as well as how well your treatment is progressing. Hope that helps. God bless.
Hi Dr. Jill,
Do you know if mast cell activation can cause fat malabsorption? I had a 24 hour stool test come back positive for fat malabsorption but my stool elestace test was normal and hydrogen breath test was also negative. So it seems like it is not due to pancreatic insufficiency or SIBO. I also had a normal abdominal CT, colonoscopy and endoscopy so they don’t think it is crohn’s or UC. No classic gallbladder symptoms either so they are not sure what is causing the malabsorption. Mainly I have weight loss, diarrhea and left lower abdominal pain. I also have ehlers danlos and possibly pots. Thank you so much for your time! Chris
Histamine affects the gut in various ways, including increased intestinal permeability and inflammation
Hi Dr Jill
I had an IVIG treatment for chronic Lyme disease and about 10 days later I broke out in hives and itching. The doctor who administered the IVIG said I had MCAS. I’d never heard of it so I did a lot of research and found your site. I was on two antihistamines twice a day for a few weeks and eventually the rashes and itching went away but, around the second week of antihistamine treatment, I noticed acid coming up and my stomach was gurgling. I now have abdominal pain off and on as well as muscle pain in my back. Is it typical for this syndrome to travel to another part of the body when the skin rash gets better?
Unfortunately mast cell activation symptoms have the potential to affect many parts of the body with various symptoms
Dr. Jill,
Father to two year old with EoE. I noticed you mentioned that EoE may be associated to MCAS. I am curious as to your connection of the syndrome and the diseases (eosinophilic types) that typically are reactionary from IL-5, IL-13 and IL-33 proteins. Is it possible that the underlying factor is the CAPN-14 gene or other genes usually associated to a specific organ tract? Or is MCAS associated with another gene and those organs? I have felt that histamines play a big part in EoE but I haven’t seen the scholarly connections between the two (H-1 and EoE).
Hi GMC – there is an association with histamine issues/mast cell disorders and EoE. Check Dr. Theoharides work for possible references..
Warmly
Dr Jill
Hi Dr. Jill,
Thank you for your article. I am wondering if MCAS can be triggered by extreme adrenal fatigue? My daughter suffered with all of the symptoms of MCAS and we were searching for a practitioner to help her with this when we ran across information on severe adrenal fatigue, which has many of the same symptoms as MCAS! Fortunately, treating her adrenal fatigue has stopped the symptoms of MCAS as well! No more daily hives! She is basically having salt daily and nano liposomal Vit C and starting glutathione. It’s amazing how much the salt helps!! So, just curious if there is a connection between these two issues? Thank you!
Hi Madeira,
Yes, fatigue is a common part of MCAS. It can result from many reasons.
warmly
Dr Jill
Is your daughter still free from MCAS symptoms by treating her adrenal fatigue? I keep thinking it’s a case of the chicken and the egg.
Hi Dr. Jill,
Is there a specific probiotic product you would recommend for those with mast cell activation?
Thank you!
Chris
Hi Chris,
There are many things listed and it can be trial and error. One of my favorites is Neuroprotek – call 303-993-7910 if you would like to try it.
warmly
Dr Jill
Hi Dr Jill,
Quick question, I have lyme and mold (mast cell) and MCS and when I treat either lyme or mold I go into anaphylaxis. How can I get better if the tx causes the immune system to flair so drastically each time?
Thanks for your time,
Lexi
Hi Lexi
You may need to work on gentle detox before your body can handle treatment
warmly
Dr Jill
What would you consider as a gentle detox? Sweating? Oil pulling?
Thank you so much for your response!
Epsom Salt baths, herbs specifically that help with detox. Check out Burbur-Pinella Detox (tincture) from NutraMedix. There’s also Red Root, Milk Thistle, etc. Just be careful by going slow and adding only one supplement at a time, maybe take it a a very low dose and build your way up as tolerated (it may take you weeks). Then, possibly add the next supplement. There are a lot of ways to gently detox. You may want to find a good Naturopathic Physician in your area.
I am the only one in my family that can’t handle the side effects of Synthroid. I get jitters, balance problems, and dizziness. I used to be on antidepressant but since I been off of them, all these symptoms happened. Still suffering almost 4 years now. I wake up with jitters, then it subsides when I get up. I take Synthroid, then Lorazepam, wait an hour, eat breakfast and take Lisinopril (bp meds). The BP meds stops my heart racing and blood pressure going up from the Synthroid and the Lorazepam stops the jitters. When I wake up in the morning the BP meds and Lorazepam worn off and very bad jitters in the am. I got thru this cycle everyday. I feel the Synthroid causes my balance problem because back in 2007 I was on 150 Synthroid, was too high so they lowered and was fine, but was on antidepressant. The BP meds causes me dizzies cuz I never was on them in 2007, just had balance problems with no dizzies. Today for the past 3-4 years both dizzies and balance problem. I hardly go out and need to stay on very low sodium diet to get less dizzy. If my BP reaches 105/65 and over, the dizzies get bad. Before ever on BP meds I used to be 120/70 with no problem. Now it feels like high blood pressure. I hate BP beds, makes me worse. I need help so bad, I don’t know what to do. My psychiatrist wanted me to try Zoloft but scared cuz of possible hallucinations (not one of the common side effects, but I fear it) and dizziness where I have dizzies already. I don’t know what to do. Why can’t I handle Synthroid? 🙁
HI Josy
Everyone is different and you may be sensitive or allergic to excipients in the Synthroid. You might try a glandular thyroid product, like Armour or Naturthroid or a clean version of T4, like Tirosint.
warmly
Dr Jill
Very helpful and informative article, but I am stumped as to why the only options listed for insomnia ( both onset and sleep maintenance) are benzos. No other effective options?
I recommend Kavinace or Kavinace UltraPM
Also Mast cell is associated with Ehlers Danlos Syndrome, or EDS
yes there may be an association
The route cause of most of these symptoms and syndromes 61 different strains of the Epstein-barr virus and 15 different strains of the non rash shingles virus. Medical science and Medcal Research cannot test for almost all of these 90 different strains and they are all viral infections. They are the underlining cause of Lyme Disease as well. Google author Anthony William and his book Medical Medium released in November of 2015. Lyme is not bacterial is an incredible claim to make and the detail in which the statement is presented in the book will unnerve those in the Lyme community because they traveled down the wrong road for the last 40 years.
I agree with this 100%! I am reading his book now!
Hi Dr Jill
I suffered an anaphylactic reaction to contrast media and iodine that messed me up. I was perfectly healthy before this and now got so many symptoms excersize intolerance, digestive issues, skin changes, loss of collagen in hands feet, it even gave me a dvt in the leg. I was so healthy before this and I marked off I was allergic to hey when I went for the cat scan. Can you reccomend what type of specialist i might want to see.to get tested. This happened to me four months ago in my home. It was a delayed reaction and it happend like three nights in a row i had no idea what was happening to me. I appreciate suggestions you can give me
Mike
Hi Michael,
You might try an allergist or immunologist who treats MCAS. If you are in Colorado you can try ImmunoE health
Wamrly
Dr Jill
Hi Michael,
I had a CT scan with dye contrast and delayed reaction in December 2016 and have since suffered greatly from all the symptoms you mentioned. The worst being the burning skin and anxiety. I am trying to find a doctor to help me. I hope we get help. This is not humane all the suffering.
Jo Anne
Hi JoAnne,
You might try Dr. Theoharides
warmly
Dr Jill
I too had a contrast dye reaction (10 hours after the scan) of intense flushing, itching and burning – it has been 4 months and I am still almost constantly reacting, have lost so many foods, trying different MCAS treatments but still struggling to find the right dose and blend. I am seeing Dr. Afrin so hopefully will get answers. But the triggering of the CT contrast dye is absolutely what kicked off this bad flare.
Hello Dr. Jill,
I am new to this. My 4 year old has been having reactions that have increased over time: flushed skin, all over itching, cough, dark circles under eyes, joint pain, constant stomach aches, irritability…etc.. She has been allergy tested for specific foods, molds, pollen, etc. All negative. Yesterday, her allergist discussed MCAS as the probable issue we are encountering. Our next steps are to monitor and observe the foods she is eating and find the triggers and avoid them. (including activity and stress or frustration triggered symptoms have been observed.) In the mean time she is to take Zyrtec daily or Claritin, (this does not seem to make a difference.) and stop back in 6 months.
I would like help in deciding what our next steps should be? What type of specialist(s) should I reach out to? I would like some more secure answers and treatment. I want confirmation that this is indeed what we are dealing with. I want consistent effort in her care. I want alternative options for diagnosis and treatment. I need some more support and resources. I am not confident in our current healthcare providers do to their lack of urgency for such a young girl to be experiencing MCAS. What can I expect for her/us? will it continue to get worse? Is this precursor to something more?
Your article and responses to others’ inquiring have so far provided me with more awareness on MCAS.
Thank you,
Amanda
A very concerned Mother
Hi Amanda
You are best finding an immunologist or allergies familiar with MCAS. If you don’t have any luck, try a functional medicine doc.
warmly
Dr Jill
Hello madam….
This is Ravi…. suffering from chronic urtic area since 4 years….. i have ring shaped hive on my skin after tajing food,and some times it comes at any time….. i have met may dermatalogists but there is no use….
What can i do….? How can i get rid from this hive…….
Pls help me…..
Waiting for ur reply mam, pls give some suggetions…..
Now am taking EBAST 20 MG….. BUT THERE IS no use…..
Pls pls pls pls…..
.
Hi Ravi
You may need combinations of antihistamines listed in the article to get control
warmly
Dr Jill
hi! just thought id add that POTS is actually postural orthostatic tachycardia syndrome NOT postural orthostatic hypotension 🙂
Thanks, Sophie! Just edited 😉
Thats alright! i’ve been having many of these issues myself for the past year. i can break out in rashes on my chest and or face and sometimes arms,i never know why. but recently i’ve realised i normally have face rashes,my resting hr is high of 120-125bpm,which flares my POTS symptoms. I feel nauseous,dizzy,the rashes can be itchy sometimes,i have IBS aswell and its normally after i’ve eaten food and weirdly enough,does not always happen the same way or always with the same food. I reacted to some food additives one day i believe and then a few days later i had something to eat with the same food additives and i didn’t have a reaction to that food. there are some things i’ll react too continuously eg. alcohol and such and alot of foods,such as apples. but some times,its really a mix and match of what i might react to that day. I’ve always had that though,just lately noticed the rashes and the tachy resting heart rate and very sick feeling all happen when ive eaten something my body decided not to agree with and even suffer with chronic reacurrent utis (looking into IC perhaps soon as we cant find a reason for it to be happening)
My question is,i’ve always developed intolerences to things/allergies after a few months of eating/using them and then i always get continously sick if i have them after this has happened. then i wait a few months i try the same food again and then sometimes i can be completely fine or get very sick.
I’ve been considering looking into Mast Cell but always thought that you have to react to something each time,is this what happens? or can it be just completely random luck?
Dr. Jill,
Someone mentioned to me that my 7 year old daughter’s “sun allergy” may be due to MCAS. I looked it up and found your article. We have been dealing with eczema issues already for mainly the past few years. We are working with our integrative pediatric practice to try and figure out her root cause. She just had blood drawn for the ALCAT this week. I have always questioned mold. How can we know if our house has mold or even her school? Can you give me anymore information on this sun allergy? This just started in October this year at the same time she was taking some homeopathic metals drops from a Functional Dr we were seeing. Thank you so much for your help!
Hi Jamie – Solar urticaria may be a sign of another autoimmune disease, like lupus. I suggest finding an integrative or functional medicine expert to help check her gut and nutritional status and screen for autoimmune disease.
Warmly
Dr Jill
Hi I’ve stubbled across your paper on a bid to try and work out my symptoms and the fact that my body seems to be on self district ‘re reactions. I first started with latex reactions after dentist visits as a child. By my teen age yrs this was blisters and swelling. This in years since has lead to reactions to fruit mainly and some spices. In the last 2 years I now after a major rection to the dentist environment children being treated. They gave me a anti histamine which I also reacted to. I’m now left that I react going into hospitals and have fits
Direct activation of mast cells by which of these :
drugs or food ? And why?
Thanks in advance.
by both drugs and foods and hormones and toxins and many other insults
I have suffered with Spontaneous (Idiopathic) Angioedema and Urticaria for more than 8 years. Facial swelling to the point of disfigurement and hives on my torso the size of dinner plates. I was tested for Hereditary Angiodema with results being negative. I was put on a regimen of Hydroxizine, Allegra and Zymetadine. While heavily drugged, I still had occasions of hives and facial or extremity swelling.
I was put on injections of Xolair every 4 weeks (150 ml) and haven’t had any symptoms for more than 8 months.
Anything else new for treatments?
Hi Mary, unfortunately mast cell issues may be trial and error of what may help… keep trying, don’t give up
We sound the same, I have had chronic hives going on 5 years and have been on Xolair for 3 or 4 years now. I also get two 150mg shots every 4 wks. It was a life saver for me as all the multiple other meds I was on at one time stopped working. I went to the ER covered head to toe in hives with trouble breathing. Epi and steriods did nothing, where in the past they worked. The ER then sent me away since they didn’t know what to do (scary situation) and told me to go see my regular doctor. I was super close to driving to MAYO clinic that day. Luckily I was referring to a dermatologist who had one 150mg of Xolair and asked me if I wanted to try it (he had not given it to a patient before), I was desperate at this point and told him to go for it. Within 4 hours in was completely clear of hives.
Dr. Jill,
I researched MCAS at the recommendation of a physician friend. I told her that my allergy symptoms have improved significantly with Zantac, Xyzal, and a Pulmicort nasal rinse in just one month. This is the first December in sone years that I haven’t had a sinus infection the entire month. Not to mention I have suffered throughout the entire year. Do you have any specific insight about repeated sinus infections? Thank you!
Hi Melissa,
Yes, the diagnosis of MCAS is made based on clinical symptoms of mast cell activation and response to treatment. So it is quite likely that your symptoms are in some way related to mast cell activation.
Warmly
Dr Jill
I have had over a dozen anaphylaxis episodes, 4 that have ended in intubation, and am on continuous infusion Benadryl using a CADD pump. My specialist has left MN and I am having a very, very hard time finding someone to accept me as a patient, is there any chance you have a recommendation for the state of MN.
Hi Beverly,
you might try Dr. Lawrence Afrin or Dr.Theo Theoharides for MCAS experts.
Warmly
Dr Jill
Hi Jill
I’m reacting to everything, even things I was fine with a month ago. I’m trying to start H2 blockers but I’m even having difficulty with that. Any ideas what I can do?
Many patients with MCAS must get compounded cleaner version of the H1 and H2 blockers or Ketotifen
Dr. Jill
I’m wondering if this might be my.problem. I have had chronic hives for going on 5 years with no reason why. I’ve taken a multitude of meds to control them..including 2 years of steroids mixed with other meds, finally they have me on Xolair, two shots once a month to control, although I still have break through hives. Could Mast Cell be the cause of this. I’ve had a partial knee replacement at 36 (March 2017), we were thinking due to the extended use of steroids (broke down cartilage). I also have a multitude of other weird issue. And I need to find out what is wrong with me… Thank you
Hello, Thank you so much for your article on MCAS. I have been trying to get symptoms under control for awhile. Wondering about palpitations. They were not mentioned here, but I have read in other places palpitations are common in MCAS. I have had many heart test and have been told by the cardiologist he is not concerned as there is nothing wrong with my heart. Wondering about treatment for palpitations that worsen when eating or very hungry. PPI’s make the most difference – symptoms much less severe, but do not elevate them completely. Oral ketotifen (1mg twice per day) helped the first few days, but then stopped.
Palpitations are not uncommon in MCAS…
I have adrenal adenomas so was worked up for Pheochromocytoma as I had heart palpitations, tachycardia episodes (10 hr long one after contrast dye) and flushing. Blood work ruled out pheo. I have had before all this started an unknown origin rash under my arms that has now spread all over my stomach and starting on the inside of my legs. I have mentioned this rash to my Dr. 3 times but he said he was more focused on the other issues at hand. Is MCAS a possibility?
Dr. Carnahan,
Thank you so much for the information that you’ve provided. Is premenstrual dysphoric disorder (PMDD) also tied in with MCAS?
Mast cell issues can certainly contribute to dysmenorrhea, menorrhagia and PMDD…
Hi Mel,
Mast cell disorders may be associated with menorrhagia, dysmenorrhea and PMDD
warmly
Dr Jill
Have gone in circles with rheumatologist and family doc. Knees get watery, pain, unable to walk in a flare up. Thought dysautonomia was the culprit. Also started histamine blockers. Went to DNA expert. Told they could test for that but not treat, went, was told hearsay of my genetics and possibilities and testing was waived. Seen there is a DNA test for MCAD. Kinda sore the experts railroaded me, presumably to set an example for going over the family crackpot. Any feedback is good. Jill. Thank You… Robert in ILL.
Hi Jill,
Love your article and can’t wait to show it to my hematologist and PCP. I just had a bone marrow biopsy and it was normal as I suspected. I have been diagnosed with multiple things that are on your list. I don’t get hives or a rash but I get this awful burning sensation from head to toe followed by nausea, vomiting, diarrhea, and horrible sharp pain in my abdomen. Sometimes I get a headache. I have been on Zyrtec and montelukast for several years. Started having major flares starting last fall that kept sending me to the ER. I had stomach surgery in November due to failed nissen fundoplication which was undone and a Linx device was put around my esophagus. Since then I have only had one major flare and I think fewer flares is due to not being able to eat very much. After this last flare a week ago I added Zantac 150 mg BID and it is helping tremendously. I still get some burning sensations and stomach cramping with diarrhea but it has improved. I have experienced anaphylaxis 3 times, 2 to medications and once to CT dye. I am trying to convince my doctors that I have MCAS but since my biopsy was normal they say there is nothing wrong with my mast cells. Where I live in Colorado there are no specialists that I am aware of. Do you know of anyone on the western slope who treats mcas? Thank you so much. Cindy
Isn’t ondansetron primarily for nausea? You have it listed under diarrhea.
Yes, it can be used for both
Hello Dr Jill- Great article! Do you see geographic tongue regularly in your patients with mast cell/candida/mold/Lyme? many people have this condition and it will flare every time there is a histamine release but I do not believe histamine alone is the cause it just makes it worse. Curious if you were able to successfully address this and if you could please share what has worked I would be grateful. many thanks!
Niteen
Hi Niteen – find and treat underlying food sensitivities, nutritional deficiencies, and toxic exposure, dysbiosis, etc
Dear Dr. Jill
Thanks for a great article!
I wonder if U have ever heard of Familial Mediterranean Fever? I take colchicine for it and thought I had figured out my life long periods of illness but then stumbled upon histamine intolerance and MCAS etc….. both of these “diseases” have many of the same triggers and share so much in common I believe they are connected somehow but cannot find any medical references to support my theory. Just wondering if U had any thoughts?
Thanks so much
Kat
Hi Kat,
Yes, Indeed, I have heard of FMF and it can be associated with MCAS, you are correct
warmly
DR Jill
Good afternoon my daughter has all the symptoms allergist thinks she might have MCAS she’s been in and out of the hospital getting worst doctors at the hospital says it’s mental becasuse when she’s having the attack high blood pressure instead of low blood pressure. What’s your opinion.
You may need to consult with an expert in MCAS
Hi Dr Jill,
Thanks for the detailed article!
If I were to lessen my toxic load (Mold, Virus and Candida) could my mast cell issue go away?
I have the same question?
Thanks
Denise
Yes, decreasing the triggers to mast cell activation may help!
Hi! Thank you so much for this article. I have Endometriosis and chronic fatigue alone with migraines and chronicle inflamed sinus glands. All diagnosied. I have a history of hives, skin irritation (now rosacea), sensitivity to foods, abdominal pain, swelling, itching, and heart “flutters”. I have seen specialist for almost everything but now would love to talk to someone more about Mask cell disorder. It was something that was brought to my attention in an Endometriosis Group. I live near Seattle and would like to make sure I am seeing a dr who knows what they are talking about. I have had 8 surgeries in the last 4 years and am exhausted and want to feel better. Any suggestions of a great dr in my area? Thank you so much!
Hi Kaitlin – try searching for functional medicine providers at http://www.functionalmedicine.org by zip
Hi Kaitlin,
I too live near Seattle and am just starting to look for a doctor familiar with MCAS. Any chance you found someone yet who you like?
you might try http://www.functionalmedicine.org or Dr. Theoharides
B”H
Dear Dr. Carnahan:
Thank you so much for all the information and insight you provide in this article. I have a particular question to ask you in regards to heparin testing, being one of a very sensitive and specific markers of mast cell activation.
Laboratories that perform heparin testing, usually do Anti-Xa assay. However, they would like to know, if there is a need to measure fractionated vs unfractionated heparin (UFH vs LMWH). Which assay is most appropriate and relevant for MCAS/MCAD diagnosis?
Thank you in advance.
Where do you go to request this kind of testing?I saw a Primary care doctor recently that suspected I had histamine intolerance but didn’t offer any testing or treatment.I seem to have chronic health problems but with no answers to what the cause is. Do I bring this up to my new primary care doctor?I am on Medicaid and they don’t want to do much testing to keep costs down.I have complained about many of the symptoms that are on your list for the syndrome,but my doctor likes to shrug them off.
Hi Jennifer – many can be drawn through LabCorp or Quest Diagnostics or Mayo clinic but I don’t know of any one lab that does all of the testing
warmly
DR Jill
Hello Dr. Carnahan,
So I am not going to bombard you with my medical history, clearly the fact that I am reading your article already tells you that I am having some issues, I am seeing a functional doctor but they are not the most informed in my case. I have a few questions that I would really appreciate you answering for me.
1) Lets say you have a new patient that can’t afford functional testing, what testing would you recommend the patient do that insurance will cover to get the ball rolling?
2) The same patient has tested positive for SIBO, IGM Positive for Yeast. This patient is sensitive to histamine at the moment. What would recommend testing with first as far as treatment is concerned?
3)Going back to question 1, what bugs should be tested for as well with the same financial restriction?
MCAS is a clinical diagnosis, testing is only a small piece of the picture
Hello Dr. Jill,
I would like to share our 15 yr old daughter’s story in the hopes of finding answers of some kind. She is on state insurance (CHIP) here in PA and I am not able to afford taking her to a specialist out of state. Our daughter, Adie, became ill last December (2017) with two weeks of what they thought was the flu (and treated it as such). She remained ill through January and into Feb, off and on. In late Feb. she got so sick that I took her to the ER where they thought she has mono, but it was negative. Her liver numbers were slightly elevated and her neutrophils were too low so they admitted her to Penn State Hershey Children’s Hospital. She remained there for three weeks. Over the course of those three weeks she had episodes/flareups that included red, flat rash on her cheeks (and upper arms and inner thighs), hot/cold flashes, fevers (anywhere from 99 to 105 at one point) accompanied by cold feet, weakness, dizziness, dry and harsh cough, sore throat, headache, abdominal pain, diarrhea, joint pain (all over but most severe in hands), swelling of face (especially around eyes), pain in eyes, shakiness, brain fog and more that I am probably forgetting.
She was seen by every pediatric department , including infectious disease and they ran test after test and couldn’t come to any conclusions. Her WBC was low, sporadically, too. After three weeks, they had no answers and she “seemed” better so they sent us home. We continued seeing infectious disease until her neutrophils went to low normal and they discharged her from the Hershey drs. in June.
Since June she has had episodes/flareups/crashes off and on. She often looks extremely pale and needs to sleep a lot. The rash on her cheeks comes and goes as does the puffiness in her face. She continues to have joint pain, as well. Over the last three weeks she has been having these episodes quite often and I finally took her to our pediatrician last week. She had us get blood work and it shows low hemoglobin, low ferritin and low IGA Antibodies. She ordered a Celiac Biopsy and that is scheduled for Nov. 7 as well as an immunology appt (both at Hershey). Other than that, she said our daughter is a mystery and to get rest and drink plenty of water.
On Saturday night, we were at my SIL’s birthday party (lots of food) and on the way home our daughter crashed in the car. By the time we got home she could not walk and was having a full blown one of these episodes. She was crying and crying that she just wants to be well again and not be sick anymore. Her face was twice it’s size, the rash was back and all the other symptoms that come with it. She fell asleep and when she woke up Sunday morning she still felt terrible. She went back to bed and slept all day. I took her to Hershey ER and they checked her for dehydration (she wasn’t), did a simple physical, told us that bloodwork was just done last week (CBC) and that they didn’t think they needed to do it again and sent us home.
Please help us. I suspect that this might even be familial as I am 43 and have suffered from joint pain, migraines, depression and anxiety (both of which my daughter has), severe nightly itching (all over– like a burning, intense itch), severe allergies (watery eyes, cough, sore throat) year round, chronic sinusitis and chronic bronchitis, fatigue, weakness, etc, for YEARS. I have had drs argue whether or not I have fibromyalgia but have never found relief or help and I usually just take Benedryl and pain relievers to try and help.
More than myself, I just want our daughter to be well. I feel like drs are telling her this is all in her head now and that she “looks ok” so she must be. I feel like because they haven’t found anything they are giving up looking at all. She has given up so many of her favorite activites and she homeschools now because she never knows when an episode will hit or how long it will occur. She desperately wants to be a normal kid again.
We are a low income family and she has state insurance (CHIP) which limits us to who we may see for treatment. I just don’t know what to do anymore. Thank you so much for your time and for your website.
Sincerely,
Ann Marie Miller
York, PA
peachpie2126@yahoo.com
Hi Ann- so sorry to hear about all that you have gone through with your daughters health. I suggest searching for a functional medicine doctor near you to help – http://www.functionalmedicine.org.
warmly
Dr. Jill
Dr. Jill,
The only period of time in my life that I experienced severe mast cell disorder symptoms was from early 2013 through early 2018. The worst sympyoms were large wheals on my feet, ankles, legs, wrists, and buttocks; also, severe brain fog and feeling drowsy all day despite good sleep at night. There were other symptoms, as well.
Through trial and error “sleuthing”, I found out what the causes were, and was able to eliminate the MCAS-type symptoms.
1) Excess oxalate deposition in soft tissues and bone, throughout my body. It happened in part due to leaky gut caused by….
2) Intestinal parasites!
3) I also found out, through detailed testing, that I was severely hypothyroid!
4) Severe, long-term hypothyroidism also had a deleterious effect on my adrenals.
5) Also, post-infection SIBO was part of the problem.
By dosing the right kind of thyroid meds, going on a low oxalate diet, using adrenal cortex supplements, most of the MAST cell symptoms went away. Now, I am addressing the parasite and SIBO issue.
It takes testing and detective work; but the root causes of disease can be discovered and fixed.
I am on h1 and h2 blockers and that helps me a lot. But I still produce too much stomach acid probably from chloride issues in food.
Can you combine h1 and 2 with proton pump inhibitors or should you use one or the other?
Imam sure of not having too little stomach acid as I tested with HCL which made my chloride food problems even worse.
I produce a lot of mucus, coming from the nose when my chloride level up and anything that increases stomach acid gives me trouble and makes my hair fall out instantly. ( also tapwater)
Yes, you may combine H1 and H2 blockers
My question was of I can combine h1, 2 AND proton pump inhibitors
I already combine h1 and 2 but my stomach I react on everything that has chloride in it ( so that woild be all food practically)
So can I combi levocetrizine ranitidine AND omeprazol?
TIA
Yes, you may combine all three if symptoms are severe. Best to speak with your doctor about dosing…
Hi Dr. Jill!
I’m just now coming across this whole mast cell world. My symptoms seemed to have started when I was pregnant with my third child. (This is what sent me on the research path.) but now that I look back, I can see other times in my life that some of these symptoms may have existed…mainly anxiety, random hives, GERD.
During my pregnancy, I started developing strange attacks after eating. My heart would start racing, i would get flushed, dizzy, and my anxiety would shoot through the roof. I would also get heart palpitations. I went to the ER twice. Everything was fine except both times my potassium was low.
I am 3 mo postpartum, and I have seemed to have developed food allergies or sensitivities. I seem to react to everything quite honestly. Mostly I just itch after eating with some asthma like symptoms. I’ve put myself on a low histamine diet, and not only am I not consuming the amount of calories needed to support breastfeeding, I feel like it’s just not working.
I don’t know where to start. I suspect I could have SIBO too. But everything is so closely matching. My husband was treated for Lymes years ago. The house we live in now did have mold that was removed. I have had more than my fair share of emotional trauma within the last year, AND I am post partum. I am a basket full of possible root causes.
My main questions…what do I treat first?
Of the main natural treatments, what are those safe for breastfeeding mothers?
Probably best to find a good functional medicine doctor who will check for infections, toxic load and activation of mast cells and treat these issues. I suspect the mold exposure was a trigger to your current symptoms.
warmly
Dr Jill
Dr. Jill,
I have “bouts” that happen without warning, usually after eating where my hands start to itch, skin gets hot/flushing, and almost immediately after is simultaneous vomiting and diarrhea, and a feeling like I am going to pass out. It is happening more frequently and getting worse. The most recent event was earlier this month and I was so dizzy I couldn’t even walk. I had to lay in bed and was even finding it hard to breathe. This started about 22 years ago during my college years and would happen once every other year or so but now it happens several times a year. This year alone, I’ve had it happen three consecutive months in a row. I have noticed that terrible anxiety can also be a pre-curser. The last time it happened I literally thought I was going to die.
What do you think this is? What should I do?
Dr. Jill,
Are you aware that many of the drugs you suggest for MCAS: Either block DAO, HNMT, or liberate histamine eventually leading to Histamine Intolerance and eventually MCAS?
I would love to hear your thoughts!
Thank you
Hi Jon
There is certainly no perfect options but some symptoms are severe enough that drugs are appropriate to control symptoms.
Warmly
Dr. Jill
Hi Dr. Jill,
I’m trying to decide if it is worth looking into MCAS for my digestive problems or not. When they flare up I have lots of digestive problems, fatigue, tingling hands/feet, low iron, migraines, joint pain, muscle pain, raynaud’s, sinus problems, and all over itching. But I don’t normally have a rash! (I have occasionally in the past, but it isn’t hives). It’s just this odd sensation of itchiness across my entire body. I’ve eliminated all of the foods that I know of that trigger symptoms, and that has greatly reduced my symptoms. But I still commonly have GERD, occasional diarrhea, sometimes fatigue, and some joint aches. And I feel like I have this low(er) level problem that I just can’t solve. Does this sound like it could be related even though I don’t really get hives?
thanks!
yes, this is possible… you may try some of the testing listed or see if antihistamines relieve your symptoms
Thank you for this information! My son, who is 28 has had GI issues for some time. He’s doing better now but he has to take Creon as he does not produce enough pancreatic enzymes. He gets hives pretty much every day. At first we thought it all came from Lyme some years ago but he was treated for Lyme. Then we came across some information about long term side effects from the acne drug Accutane. We think it may have more to do with that. My question is, he currently is taking something called Antronex by Standard Process which is yakriton that a NP doctor prescribed. He also takes D-Hist by Ortho Molecular. I saw you liked Umbrellux. Is this a better fit for hives? Do you know about Antronex for histamine? I still believe there is a connection between his GI symptoms, the pancreas and the hives and that he can be healed. He has improved with eating a very clean diet and lots of various supplements. I just know from reading about histamine that it’s not good for his gut. I would be curious if there’s a better supplement for the hives. Know anyone great in New York City? We’ve been though a few trying to find someone smarter and more dedicated.
Hi Alisa
For hives or allergic symptoms, I prefer Thorne Quercenase or NeuroProtek
Warmly
Dr Jill
my daughter was diagnosed with a solitary mastocytoma when she was 6. She has had issues right along with NSAIDs causing full body rash. as a teen, she started having issues with peanut butter causing a huge gi flare and urgent bowel evacuation. She has since developed rashes with other foods. Her whole life eating has caused facial flushing, which has gotten worse. She has been on antihistamine and took herself off 7 months ago. since this time all of her reactions are worse and now she is experiencing headaches, fatigue, flushing, achy body, depression, and anxiety. First of all, can a solitary mastocytoma turn into mast cell activation syndrome? or what else could it be? (her father was diagnosed with MCAS 5 years ago) Second, do those symptoms seem like they point to a mast cell issue? Her ANA was high, but every other test to point towards autoimmune was negative. We are in an MCAS ignorant state and we need to figure out the direction to go. Her new primary care is willing to learn and help us, I just am not sure if this is the right direction to look. Any insights would be appreciated.
Not even sure where to start. My 34 yo son has had several flare-ups game f hives and swelling/inflammation over the last 25 days. Even ended up in ER twice. To date they’ve told him autoimmune or allergy. He’s been taking prednisone and it totally disappears. As soon as he reduces the amount or quits, it totally flares. Also totally drains him. Allergist wants him off the prednisone so he can run tests, but both times he’s stopped, he had a major flare/up. Considering finding a different doctor or hospital with more experience or research with mast cells. We live in Michigan, so considering Henry Ford, U of M or St Joseph Mercy. Any thoughts?
Dr. Jill,
thank you for this article. I started my journey with this nasty condition about 1 1/2 years ago. Since the first reaction, my life has been dramatically changed, as anyone with this condition know. My doctor is a specialist in the field, and I have even him stumped. How can I go about finding a doctor strictly for mast cell disorders? My immunologist believes MCAS is what I am dealing with, but he doesn’t have to testing capabilities where he is located. Any help, advice you can offer will be greatly appreciated!
Thank you for your time!
you may try Dr. Afrin or Dr. Theoharides, both MCAS experts!
I saw a GI in Houston, TX. When she did my EGD, she stated she saw a lot of mast cells in my upper small intestines. We also did a DNA/PCR stool, which came back for high levels of candida. She said I have mast cell activation syndrome. She started me on Diflucan 50mg qd x 2 weeks. I have been sick since 5/2018 with diarrhea, nausea, vomiting, severe bloating, abdominal discomfort, headaches, severe brain fog, fatigue, fever, severe bile and acid reflux. I did inquire with her to do the 24 hour urine, serum tryptase, and bone marrow bx. She says I need to f/u with an Allergist. I also inquired with my PCP, and she says that is out of her scope of practice. I have reached out to physicians with The Mastocystosis Society and some physicians will not see you unless you have all these tests completed while others specialize, like only mast cell leukemia. I do not know where to go from here. Any help would be greatly appreciate. Lola Normand
I have mast cell activation disorder and chemical and electrical sensitivity and mold toxicity.what do you think of using allergdhq for histimine..and please tell me how I can get some toxins out I’m very toxic they are cropdusting here and I can’t handle it..my nose stays dried out and my eyes burn and feel weird and I taste metal and have no real teeth Left..always have that taste..and lymph always backed up and have yeast
Please reply to me by email on my last comment
Hi Dr Jill,
Thank you for the very informative article. I am in the UK and there seems to very little knowledge or acknowledgement of MCAS here but I suspect my son has it. He is 3 and has had symptoms from 4 weeks old. He is diagnosed with an ige latex allergy, non ige food allergies and probable Histamine Intolerance. He suffers GI issues (vomiting is under control but still suffers mucus diarrhea a lot), skin issues, (itching, flushing, hives, (negative to ige allergies), thickened red skin with nettle sting type rash, discoid eczema), chest issues (chesty cough, asthma type symptoms, viral wheezes, chest infections), he does also seem to suffer anxiety to certain situations, but this may be age appropriate. His skin symptoms have been significantly reduced since following a low histamine diet. To my mind he fulfils a number of the criteria above but our allergy specialist pediatrician has discounted mast cell involvement. Does this sound like it could be MCAS?
I was diagnosed with CFS/ME in 2010, and suffer many of the symptoms (though have never suffered from hives etc) so I am wondering if perhaps I have an underlying mast cell issue.
Are mast cell issues hereditary, could I have passed an underlying mast cell condition like MCAS to my son, but it just manifest differently?
My son’s current treatment plan is to continue to follow our low histamine diet but try increasing amine active foods, but we are failing most foods we try (even low histamine). At such a young age are any of the possible treatments you have suggested appropriate to try? (If I can even get a medical professional to consider the possibility!)
Thank you so much for your help
Yes, it is appropriate to use H2 and H1 blockers and other MCAS options in children if your pediatrician is willing to prescribe
My daughter will soon be tested for MCAS and after reading the list of symptoms I now suspect I may have it(I have EDS). Could you recommend a knowledgeable doctor in or close to NH?
The best I know of for treatment of MCAS are Dr. Theoharides and Dr. Lawence Afrin
Hi Dr. Jill,
Can you recommend a specialist in the DC or greater DMV area?
Additionally, is there a link with mold and mold exposure. A naturopath friend of mine recently mentioned that they may contribute to my symptoms.
I’m practically in tears reading this because I feel like I may have an answer to the chronic fatigue, eczema, headaches, itching, GI upset, and three spontaneous (and/or exercise induced) anaphylactic episodes that have characterized the last two years of my life.
I was told that mold definitely related. ( by 3 specialists)
Dr Jill, I LOVE your work
I have DX MCAS and terrible adrenal issues. I wake early each day with fight or flight symptoms that send me through the roof. These attacks also continue throughout the day almost every time I eat anything. I have many symptoms ( lyme and other tick diseases) but recently developed transient numbness of the skin. Can the MAST issue cause this numbness problem and this fight or flight reaction? The latter has me going absolutely insane.
Histamine and MCAS can contribute to anxiety and other related symptoms
HI Jill,
I’ve just read a large portion of this info to my husband to help him understand what might be going on with me.
We lived in a house with mold for 5 years and I was very unwell for the entire time. Multiple systems in my body were effected and sadly I went on untreated for 4/5 of those years. I discovered dr Richie Shoemakers info and began my healing journey. I’ve had a severe histamine issue the entire time and wonder if I might have been best buying shares in Zyrtec .
We moved houses, leaving all soft furnishings behind. My health began to improve immediately. Quality of life began improving over 18 months and then all of a sudden, like switching a light switch on, my symptoms came back! I went back to my integrative dr and we couldn’t work it out until one Monday morning in my classroom, I noticed a water line on my classroom carpet. There’s been a slow drip in a cupboard that over months, had leaked through a wall and into the carpet in my room. I’m 18 months on and still extremely unwell. Brain fog, anxiety, hashimotos, sleeplessness, major Debilitating gastrointestinal issues, permanent severe histermine issues – Zyrtec almost daily. Wheezy chest especially on one side. Blurred vision – even with prescription glasses.
Anyway, my work place don’t see an issue as they can’t see any mold!
I so wish there was someone who could help me. I feel like I’m slowly dying.
some Students have hives and itchy skin, brain fog.
Thank you for
I have suspected mast cell activation disorder (skin hives from sun with fatigue), and a mitochondrial disorder diagnosed via genetic testing (WES). My functional medicine provider recommended Huperzine A some time ago, and I’ve taken it with subtle positive effects. I have also occasionally taken Fexofenadine for the mast cell fatigue and skin issues.
However recently I started taking a dose of each TOGETHER, and wow! The energy it gives me is incredible and lasts all day. I don’t drink caffeine but it is what I imagine that feels like. I’ve spent the past several days researching what could be happening between those two: Huperzine A + Fexofenadine, and am coming up empty. Ideas?
I know that Huperzine A is contraindicated with anticholinergic drugs, but Fexofenadine is not anticholinergic.
Huperzine A affects levels of acetylcholine by affecting re-uptake and Fexofenadine may have some cholinergic effects as well as an atypical antihistamine (benadryl or older antihistamines typically exert anti-cholinergic effects but fexofenadine does not in studies) so I suspect you have having an increase in acetylcholine which may make you feel more focused or improved concentration. It is likely a unique effect that may also have to do with you personal genetics
I have chronic migraine, POTS and chronic intestinal issues. I feel better when I take Benadryl. Worried about long-term cognitive effects of the drug, even though my brain fog is already severe. Will run this past my doctor. Thank you, Kim
Hi Dr Jill, thank you for this article. My specialist has diagnosed me with mastocytosis, it all started with getting my gallbladder removed. I got so much worse! 4 years later, I am struggling to stay out of the IBS box, I am positive for every one of your points! So long story short, my specialist believes my gallbladder surgery triggered a mast flair. It makes sense.
I am currently trialing H1 and H2 blockers. It’s not an instant fix but I am sleeping through the night so I’m hopeful. Great article xo
Hi Dr Jill,
I was recently diagnosed with Joint Hypermobility Spectrum Disorder. There are many healthy foods which I have to avoid as they exacerbate my ligament laxity, but I don’t suffer from obvious MCAD symptoms like hives, runny nose etc. It’s only my joints that are affected. I have a bloated stomach no matter what I eat but I have healthy bowel movements. A few days ago I discovered that my stomach doesn’t tolerate teff grain and I must rinse quinoa for 15 minutes before cooking, otherwise I will vomit. I sleep well unless I am woken up by pain. I did suffer from eczema behind my knee for many years but that has cleared up. I have had both hypothyroidism and hyperthyroidism in the past. I also have severe endometriosis.
At present my joint hypermobility is so disabling that I’m too weak to leave the house. I’m trying a bovine trachea and liver supplement which is supposed to normalise the immune system. I’m having trouble even taking this as it is also worsening my hypermobility by the day.
I’m wondering what your thoughts are and whether I should try a MCAD medication/supplement.
Thanks,
Tania
Hi Tania
Many patients with joint hyper mobility also have issues with MCAS
warmly
Dr Jill
I have been suffering with this for years, I had no idea what it was. But now, after being exposed to a couple types of mold, I am way worse. I can’t exercise, I can’t eat certain food, I react to a ton of stuff. I lost like 13 pounds for not being able to eat. I treated the small intestinal bacterial overgrowth, and I have been spacing out my meals and fasting. But I’m a personal trainer and not being able to exercise consistently is killing me. I will exercise, and then the next day I am in a flare up for three days. This absolutely have to stop and I don’t know what to do. I have seen a functional medicine doctor in Pittsburgh. I got my house remediated from all mold. I threw everything away. I eat a low fog map low histamine diet. I take a lot of supplements. Cytoquel, D hist, meclazine for dizziness, neuroprotek, freeze dried kidney for dao from a cow bc I don’t eat pork. Are use my sauna every other day. I just don’t know what else to do. I really want to get back to exercising regularly. And I hate yoga. I have constant G.I. flareup no matter what I do. Constant nasal stuffiness at random times through the day. Are used a lot of oregano and silver nasal sprays to kill the mold. Which I’m still doing. I just figured I would put this story out here to see if any of you have any suggestions that could possibly help me. I really need to control the mast cell response in order to be able to live my life.
Hey Teresa ! I said this to Kay and I’ll share it here too. check out : juice fasting with histamine tolerance mcas (on YouTube) a woman speaks to this. Chemical detoxing via prolonged juice fasting / GI reset via prolonged juice fasting can help. Do this with support!!! See Alexandra cousins on Instagram or iamsiadi or find the coach from her YouTube video.
HI Dr. Carnahan. I don’t know if you are able to help me. I am from Canada and am in Florida right now on a winter vacation. Three months ago I had a severe reaction to food (and possibly environmental factors) with my face swelling and hives all over my body and loss of my voice. My husband took me to the hospital for treatment. It’s now three months later and I am still reacting to, what seems like everything, I have been taking Claritan in double doses (am and pm) since the first initial outbreak and using a histamine block when I eat anything. I’m just not sure if it’s helping or not. I’ve been a little stressed out and thought that I would use some essential oils in my diffuser and wow did that NOT work. I am burning all over with hives and I am miserable. I was on a medication to help with hot flashes (venlafaxine) which just over a month ago I found out is a DAO blocker. I have since stopped taking this medication and have been doing a histamine free diet. Now I’m freaking out …. is it the medication and it has to work itself out or is it this MCAS? I’m sitting here in Florida and wondering : do I just go home, and shorten our vacation and see my doctor or is there anything I can take to help me through this time. I would love any help you could possibly give me on this matter.
Hi Kathy
You may want to test and treat for factors that make MCAS worse, like mold exposure or chronic infections or treat underlying methylation and histamine breakdown issues
warmly
Dr. Jill
Hi Dr. Jill,
I happened to come across your post while looking for information related to mast cell attacks. I am a college student and used to play rugby, but about 16 and a half months ago, I began to get fairly sick. It was original thought that I had injured my abdominal muscles given that I had taken a rough hit in the stomach prior to all of my symptoms showing up, but it is now thought that the hit just happened to coincide with the start of all the symptoms: LUQ abdominal pain, nausea, dizziness (with & w/o vertigo), headaches, loss of appetite, chest pain, difficulty thinking/concentrating, fatigue, and anemia. Over this time, I have had at least fairly severe 3 attacks that I can remember to a “T” from overexertion during physical activity or medications (i.e. lidocaine injection). Each one seemed to exacerbate my symptoms, especially the abdominal pain, difficulty breathing, dizziness, and feeling of passing out but don’t. I have had smaller attacks associated with alcohol and bee/wasp stings.
Approximately 7 months ago, I came across mast cell diseases while researching what this could be, and it seemed to be a very strong possibility considering how I had seen numerous specialists that could not figure out what this is. I brought this to the attention of my PCM, and he put me on Claritin, SIngulair, and cromolyn sodium, which seemed to have helped but does not prevent attacks.
I have had my tryptase level tested and had a blood test looking at the C-KIT gene, but these came back normal. However, I do know that there are other compounds/gene mutations that can occur to be the cause.
One of the specialists I am currently seeing says that mast cells could be the cause given my symptoms and that medicines are effective but also that I may never get a diagnosis, which does not sit well with me because it really hinders my ability to complete certain requirements for graduation, and my school needs answers if I shouldn’t be doing certain things. If this is MCAS, what things should I be on the look out for, and what protocols (i.e. going to the ER) should I have in place in the event of an attack? I know that this is a long reply, but I would greatly appreciate any input and advice you may have.
Thanks,
Sally
thanks for sharing, Sally
MCAD is a clinical diagnosis and may present without elevated tryptase or other labs abnormal at times
warmly
DR Jill
Can you please explain why NAC is included in your Hist Assist supplement, when it is known to lower DAO? I definitely get an increase in my Mast Cell symptoms when I use NAC.
It also increases glutathione and inhibits eosinophilic response as well which may decrease histamine https://www.ncbi.nlm.nih.gov/pubmed/17456219
My son has had a sudden onset of heat induced urticaria. Not many doctors in this area seem to be familiar with it.
He tried the H1 treatment course. He has now received his first injection of Xolair. It has not helped yet. He is only two weeks post injection, so we know it may take some time.
He is only 22 and frustrated that he cannot exercise or even take a walk in weather that is over 60 degrees without breaking out in hives.
Do you recommend using your histamine blocker along with Xolair? Do you also know of any specialists in the Ohio area for this type of condition?
Thank you!
Hi Jackie
Solar urticaria may signify another underlying condition such as hypothyroid. I suggest finding a doctor to rule out other causes or consult with Dr. Lawence Afrin or Dr Theo Theoharides, both MCAS experts.
warmly
Dr Jill
Thank you! I do have an appointment for him.
He also gets the rash when he works out and sweats. Could that be from hypothyroid, as well?
Sincerely,
Jackie
Thank you so much, your articles are so spot on! I had a friend forward me your articles and it is exactly the info that is helping me understand what is going on. I have been diagnosed with cutaneous mastocytosis/mast cell disease. My family Dr. and I have worked together and seem to have it in control, but I do struggle everyday trying to figure out what my triggers are. Your article is so helpful! My Dr. and I have decided I take Cetirizine 10 mg. 1x, famotodine , 20 mg., 2x, D-Hist 1x, Mag Oxide 400 mg.(mag. was low), Buffered C-1000 Complex, Vitamin D, Panthothenic Acid 2x, Vitamin D3, MK7. I definitely don’t like taking all these, (I always prided myself, 58, and really never taken any pills except an occasional Benadryl). I am really trying to watch and eat a low histamine diet. Especially since adding the mag oxide, I feel that I am controlling my symptoms. Like I say, the triggers are still a mystery. I really appreciate the info and look forward to reading more. Also, I think I may discontinue the D-Hist and try your Hist. Asst. Do you think they are probably about the same? Once again, thanks for all the info.
Hi Karen
Yes, I like the Hist Assit and think you would benefit if you’ve previously tried the DHIST
warmly
Dr Jill
Dr. Jill,
Can exercise induced urticaria be caused by something other than allergies? My son is having no luck with allergy medicine and Xolair. He breaks out as soon as he begins to sweat.
You had mentioned hypothyroid in your last response and I am hoping his doctor will test him for this when he can get in to see his doctor.
Thank you!
It would be worth checking his thyroid function to rule out hypothyroid
You suggest that NSAID’s may be a trigger and then you include NSAID’s as a potential symptom reliever? Come on.
Yes, this is true… with MCAS there is no one size fits all and one person’s poison can be another person’s relief
I agree with you
For years I have suffered with hives and itching triggered by direct heat. (heating pad, hot water, heated car seats) For a while it was relieved by antihistamines such as benedryl but it has stopped working. If I stand for a while in the sun I break out but I can be in the sun all day if I am moving. I am looking for some suggestions.
Solar urticaria can be due to autoimmunity, hypothyroid or other causes. Best to get a work-up for other contributing factors from your physician
I just had a complete work up with my physician-everything is good. Could one of my medications be causing this? Should I see an allergist? I am on levothyroxine, losartan, atrovastatin, metroprolo. hct. clopidogrel. It’s not just the sun when I sit for any length of time-it’s heat. I can’t use a heating pad.
have they tested anti-cardiolipin antibodies?
I am unfamiliar with this. Can you give me what it is and why they would do this test? What would the test reveal? I need to discuss this with my doctor if it is a significant factor. I had a CBC and WBC. All the results were in normal range. Is there one result in one of these tests that would indicate further testing is needed and what would you be looking for?
Hello!
I was diagnosed with a “suspected” mast cell disorder and prescribed 4 10mg Zyrtec per day plus 1 montelukast tablet per day. Wanting to try a more natural approach I purchased D-Hist. After my very first dose of 2 capsules I broke out head to toe with rash and itching. Very frustrating…so hoping that the OTC meds are ok to take for long periods?
Also, are mast cell disorders hereditary?
Thank you!
Hi Susan
Some patients have trouble with bromelain but you can try plain quercetin instead if you like
warmly
Dr Jill
I was diognosed with mold toxicity and chemical sensitivity and mast cell activation disorder and hoshimotoes and yeast and cirs and mthfr and maybe heavy metals I’m always toxic from enviroment and metal taste and nonstop yeast eyes sticky and burn and in nose nonstop metal taste and yeast I think it has all given me scitzophrania I say momma outloud and not on purpose and slap myself hard in face when real toxic Dr Jill please help me the air outside bothers me and believe I’m in mold and believe I have leaky brain and gut .I’m dying Dr Jill I itch bad and get tiny scabs all over and rashes and brain gone and get hive bumps and burning skin..love candy
Hi Candy
You might try getting an air filter like Austin Air Healthmate plus – call if you have questions 303-993-7910
warmly
Dr Jill
Hello Dr. Jill,
I have been sick with weird symptoms for as long as I can remember. But over the last 15 years(with a break for a few in between) I have been having these “attacks”. They involve hot and cold flashes, rapid heart beat, burning skin and when I use the bathroom it feel like I’m peeing or pooping acid (Dramatic, but it burns bad leaving my body), feeling of adrenaline coming in waves, muscle spasms, diarrhea, severe stomach pain, inflammation in my hands and feet(that’s common most of the times) dry mouth, blurred vision, vomiting. They are varying levels of uncomfortable. Medications that cause it create a very bad attack, some foods make it worse than others. And hormones fluctuations make me believe it’s why I’m getting it monthly now, I’m 47 and always around ovulation time. I also had to have my thyroid removed … which I believe was the cause of this thing. I’ve always thought that. When I was pregnant with my second child, who is six now, many symptoms went away for a while. Weird! But they did. They all came back. I’m sick a lot. I’ve seen endless doctors. I saw one who said it sound like mast cell attacks and she gave me an antihistamine. I took it that night and had a severe reaction to it. One of my worst. Weird thing … when they stop it’s sudden. It’s just done. I don’t know who to see or where to go, but I know I’m tired of getting sick. I was sick again last night and my husband was distraught and asking me to see a doctor, but honestly … at this point with all I’ve seen I don’t understand the point. Yes I want it to stop, but I don’t think it will. I feel like I must be in perimenopause which can’t be helping this. I think that’s why I am sick so often now. Any advice? Suggestions? Know if any local doctors in Southern NH?
Thank you!
Erica 🙂
Hi Erica
I am sorry to hear about your suffering. Hormones can also affect mast cells. You may try Dr. Theoharides or Lawrence Afrin for MCAS expert
warmly
Dr. Jill
Hi Jill,
I recently started seeing a naturopath in my area for MCAS caused by mold. I’m currently working on detoxing/moving and taking quercetin. I’m on a very limited amount of food. This came on very quickly and my body only tolerates a few foods right now. Any suggestions on how to successfully add foods back in and what to try?
Hi Kristy
You might try Histamine Blocker prior to meals.
warmly
Dr Jill
I agree with you
I agree with you
I agree with you
What do you think of allergdhq to help with mast cell..I have mycotoxins and mast cell activation And hoshimotoes and yeast and metal taste and I believe marcons and detox pathways don’t work properly..and living in bad enviroment
Hi Dr Jill,
I ran across an article about histamine overload about 2 years ago & did a bit of research on my own because my primary doesn’t take my concerns seriously. I’ve taken some control by taking a histamine blocker & changing my diet. It has helped some, but it takes next to nothing to upset the balance. I need someone to tell if this is what I’m dealing & to help me chart a clearer path to better health. I’m sick of the overwhelming fatigue, headaches, etc. I’ve been to two functional medicine practitioners in my area with mediocre results. Any suggestions?
I am 61 and have suffered from what one family doctor decades ago termed “terminal wierdiitis wierdii” all my life. I have been diagnosed over the years with a laundry list of problems, including, three years ago, systemic nickel allergy syndrome. This week, I was diagnosed by a functional medicine practitioner with MCAS as well. Unfortunately, all the supplements recommended for treating MCAS are based on high-nickel plants, which I cannot take because of my SNAS. Suggestions?
Hi Dr. Jill,
I had a series of gastrointestinal issues since 2010. I was first diagnosed with h.pylori. A few years later, SIBO, then in 2015 with small intestinal mast cell. I also have stinging sensations on my skin at time. I can usually control it with zertec and singular. I just recently had a colonoscopy and had 18 colon polyps removed (March 16,2021), 8 were precancerous. I recently stared taking hormone replacement in Sept. of 2020. I really feel like my mast cell issues are more than just my small intestines. I haven’t been educated on mast cell until recently and I’ve educated myself by reading a lot. I am now waiting to hear from a test to find out if all of my colon polyps are hereditary (DNA). But one question that I have is, could me starting on hormone therapy have anything to do with maybe mast cells being in my large intestines and causing all the colon polyps?
Hi SC
Generally bioidentical hormones should not contribute to colon polyps. however hormones can affect mast cells so there still may be a connection to your worsening symptoms.w
Warmly
Dr Jill
Hello Dr. Jill,
Thank you so much for your informative article. I’ve been sick for years and have a long list of allergies. I’ve been diagnosed with gastroparesis, fibromyalgia, ibs, to name a few. I heard about this disease a long time ago, but when I brought it up to my doctors, they just brushed it off so after a while I gave up. I have a new doctor and after another reaction to a new med he tried to put me on, I suggested this one again. I’ve done a lot of research and I have all the symptoms but they’ve only gotten worse over the years. The doctors could never explain all my symptoms and link it to one specific disease and some looked at me as though I had to be lying. I have really bad allergies to a lot of food, a lot of medication, as well as air allergens. Smells, stress, too hot, too cold, too much stimulation, exercising can cause what I have termed ‘attacks’ which is where I get horrifying pain in my torso area, the muscles contracting, vomiting, diarrhea, cold chills, trembling, erratic heartbeat, exhaustion and the only thing that’s ever helped was a flexeril and a benadryl to make them stop. I have all over pain and nausea on a normal day as well as increasing neurological symptoms. I’m on a low dose of lyrica which a low dose of anything is all they can ever give me. Also muscle relaxers and two nose sprays. After dealing with this on an increasing basis from the time I was fifteen, (I’m almost 37) I’m hoping this new doctor listens to me. I may take your article with me to my appointment along with my list of symptoms. Having this information has really helped me and I really appreciate you putting this out there for people that have been suffering with this for years.
Dr. Carnahan:
I am looking for a doctor that specializes in mast cell diseases. I have mast cell activation syndrome and my doctor retired. I live in the Seattle area. Thank you so much for this excellent website.
Dr Jill I have mast cell activation and hoshimotoes and cirs and chemical sensitivity and mthfr gene and mold toxicity and staph in nose and I believe broken blood brain barrier..I’m so toxic and imflammed and stuff on skin eyes sticky and burn and in nose and throat irritated and tissue toxic and brain gone and blaceyefloater in right eye vision that stays there and moves around when I move my eyeballs and jerking and zappings on skin and heart raising and feel like I’m in sci-fi moie and eyeballs sore and say momma outloud and not on purpose over and over and randomly and other things feet numb and hands and fingers and toes cramp up sore any place you touch me and I get sharp pains and sticky lips and heat in face and have slapped myself in the face hard
Okay I am not happy to see Benzodiazepines on this list for treatments!! Tapering off those darn benzos is what gave me my Mast cells issues! Benzos are a very dangerous class of drugs that are destroying people’s lives. I work with people tapering off these drugs and antidepressants. There have to be better solutions than that. I was surprised to see this on that list.
Hi Karole,
While I agree this is not my first choice on treatments for mast cell disorders, there is no denying that it can be a game changer for those with severe severe symptoms.
warmly
Dr Jill
I came across your site after researching 100 other blogs. What natural supplements would you reccomend for someone that has salicylate and oxalate issues as well?
I can’t eat any food without 2 different DOA’s every meal. My symptoms are bruising all over my legs, panic attacks, heart beating fast, feeling like I am not getting enough breath, tingling sensation all over my head and leggs, stomach pains… I can go on. Also, you mentioned some supplements release hestimine… what are they? Thank you
Hi Jill.
I need to avoid fermented foods if I have MCAS according to you, but I’m pretty sure, that if I have it, it’s because of estrogen dominance, and foods that can bring down estrogen is vegetables and fermented foods…. So what to do? 🙂
Sincerely, Ane
Hi Ane
You can still do many vegetables that are not fermented like cruciferous and leafy greens!
warmly
Dr Jill
Could you add more information or give references on Pentosan – or consider a separate post about it? It is the first I’ve head of this for MCAS. It seems it may be used for interstitial cystitis (IC). Is it effective outside the bladder? I could really use a mast cell stabilizer that buffers cell permeability and also has anticoagulant and fibrinolytic properties!
Hi Dr. Jill,
Thank you so much for all this information!!! It sure seems I could have MCAS!
In October I started seeing a FM provider for 3 things. 1 of which is this pain on my shin that started as a bruise back in June and lasted a while (not sure I hit my leg though) and once the coloration left it remained sore with lumps around the area and random radiating pains up to knee and into foot. (thought it was this new sedentary 8-5 life). That has since gotten a bit better but comes and goes and the nodules are still there. FM feels an indentation in my shin. I also have this lymph issue in my throat below my right tonsil where I see a little protrusion with a white tip (since Feb 2019) and FM feels 2 nodules in my lymph; and lastly the issue in my esophagus where food was feeling like it was getting stuck to being inflamed at times with an almost gagging sensation and increased phlegm. Also hurts to talk when it flares up! This is my biggest concern.
My last trip 2 weeks ago I told him about the organic blueberry incident that set my esophagus off – felt like an anaphylaxis type reaction so he put me on Histamine Scavenger but never mentioned MCAS or restricted diet. 🙁
Unfortunately, my labs show HIGH Vitamin D toxicity (333!) so he put me on Quicksilver Ultra Binder and Biotics Research Multi-Mins. Is this the right way to extract it? (a local chiropractor recommended a tanning bed with D Bulbs to activate the Vitamin – but I’m afraid to try!)
My brain wants to attribute my declining health to this new job that I started mid-June 2022. From the high stress to this chemical smell in here – I’m worried it’s something in this building. I had been feeling fine up until I started this job and really about July 4th weekend is when the esophagus issue started. The symptoms got worse around Labor Day weekend and have been very debilitating. Organic Figs, blueberries, and flaxseed all make my esophagus flare up. I’ve been on low FODMAP for 10 years. Cannot tolerate the smell of garlic, onion or brussels sprouts and if I eat it my stomach gets upset and bloated. I have NO idea what I’m going to be able to eat and considering I live in a small town in Nebraska where Walmart is the only place to offer a “small” section of organic “2-day” produce I’m limited!!
I honestly have felt like I’ve been dying a slow painful death since Labor Day. No energy, brain fog, terrible tinnitus, depression over health and job, pain in my leg and esophagus and not sure I was even diagnosed properly. Could all of my symptoms be from the Vitamin D? I started back on Vitamin K – a mix of K’s and I have not taken Vit D or eaten foods with D or even Calcium since learning of this.
I was also told that I have Lupus as the ANA results were Positive – Abnormal. So I’m taking Panaxcea Autoimmue 1. I question it as he based it off 1 test and I do not have a red rash on my face.
History on the lymph – Urgent care said lymph infection or autoimmune; and go see ENT. ENT says: stay on meds it’s nothing. 10 min and out the door. It went down to where I could barely see it before I started this job (Spring 2022) and then flared up with the stress. I’m on a holistic lymph support (liquid) but not sure if helping. I also tried low level laser therapy on shin, lymph in neck and he did it on my ears for the tinnitus – which I only did once). Unsure of this method.
Also VERY sensitive to odors. I get what I think is phantosmia. Is this from MCAS?
I’m a mess and now I just had to have emergency root canal so it wiped out my health budget. It’s nonstop stress. Any input would be so gratefully appreciated!!!! I do not have food or provider options where I live.
God Bless!
Hi Dr Jill
I live in Australia and I came across your page while researching information for my 8 year old son.
He has had over the last 4 month sudden random swelling of his lips, under eye and itchy hives, that slowly build up and take a while to go away after given an antihistamine.
We have been told it’s Chronic Idiopathic Urticarial angioedema. Is this a form of MCAS? Can it occur In young kids? Is there a chance they grow out of it?
Is Histamine blocker safe for children and would it help his symptoms along side the antihistamine?
Thank you
yes, it would be safe to try in 8 years or older
Dear Dr Jill,
I was relieved and extremely grateful to be diagnosed with MCAS after 30 years of getting nowhere, I enthusiastically followed every new and elimination diet and consumed mega amounts of “recommended supplements and compounds, broth etc, trying every alternative possibility, Nothing worked. Symptoms were worsening, e.g.chronic coughing, sneezing, reflux, digestive upsets, breathlessness, itches, sleeplessness, ear ache etc etc. Fragrances of all types, chemicals excacerbated symptoms, failing eyesight, glare issues, excipient sensitivities etc.
My situation has vastly improved when I stoppped all oral supplements and Thyroxine (using Iodine on skin). Antihistamines also cause many side effects for me so not an option.
On a low histamine diet, avoiding probiotics, broth, etc. I try to eat only real food, unprocessed and fresh. Not easy, If I weaken, sleep is the first to suffer. So really have to adhere. Have to wear a mask wherever chemicals and fragrances appear, otherwise stomach turns flips and symptoms appear, Doing breathwork to counter breathlessnes and coughing. It’s sometimes a drag but understanding MCAS has helped enormously to keep me on track. One thing though, am now 68 and I have learned that there is always hope in the form of expert advice and info. So do not give up folks.
Kind regards,
Debbie B
Share: