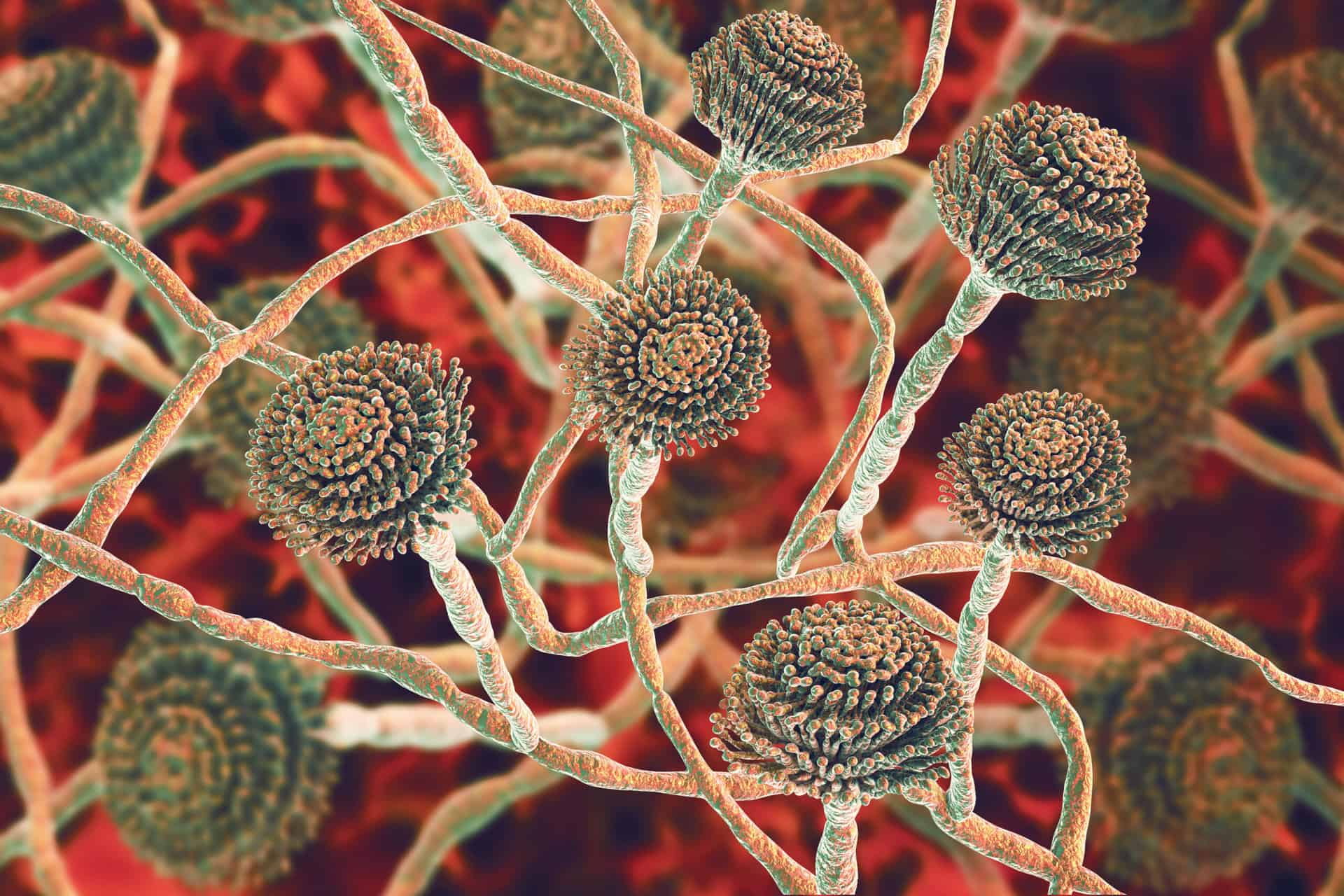
Fungus is among us. And while that’s usually not an issue, sometimes these opportunistic fungi can become problematic – invading and overthrowing our immune system and triggering a fungal infection. And to make matters worse, there’s a growing number of fungal infections that are becoming resistant to the limited number of antifungal drugs currently available for treatment.
But emerging research is finding that the secret to addressing and healing these troublesome fungal infections may lay in a tiny cellular structure known as the mitochondria.
Today we’re going to explore exactly what a fungal infection is, some common infections triggered by invading fungi, how we’re currently treating these infections, the fascinating role the mitochondria play in all of it, and most importantly – how you can best shield yourself from contracting a fungal infection. Let’s dive in.
What Is A Fungal Infection?
A fungal infection is any infection caused by a specific class of organisms known as fungi. The word “fungus” encompasses a wide variety of different organisms – with over 18,000 distinct species being identified within the kingdom of fungi. Some commonly occurring types of fungus that you’d likely recognize in your day-to-day life include things like mushrooms, mold, and yeast.1
In fact, you likely come into contact with multiple fungi on a daily basis – from fungal spores floating in the air to the yeast in your bread and from the mushrooms in your salad to the mold growing on last week's leftovers. While much of the fungi we come into contact with are harmless or even beneficial, these complex organisms can also have a much more sinister side.
If certain strains of fungi are able to invade your body and evade your immune system they can cause a wide range of infections ranging from minor and irritating to serious and life-threatening.
What Are Some Common Fungal Infections?
Some of the more commonly seen forms of fungal infections include:2,3,4,5
- Skin infections: Like athlete's foot, ringworm, and jock itch caused by a group of fungi known as dermatophytes
- Yeast infections: These infections are caused by an overgrowth of a class of fungi known as candida that can affect your mouth, digestive tract, urinary tract, genitals, or skin
- Valley fever: A serious respiratory infection that can sometimes occur after inhaling the spores of soil-based fungi known as coccidioides
- Histoplasmosis: A respiratory infection that can happen after inhaling the spores of a fungus known as Histoplasma that’s often found in soils containing high levels of bat or bird feces
- Aspergillosis: A sometimes life-threatening pulmonary infection that can spread from the lungs to other organs after inhaling spores from a type of mold that produces mycotoxins known as aspergillus
- Cryptococcal meningoencephalitis: A serious and sometimes deadly infection of the brain and spinal cord that can be triggered by the inhalation of a yeast strain known as cryptococcus neoformans regularly found in soil, decaying wood, and even bird droppings
- Mold-related illnesses: Chronic exposure to certain strains of toxic mold can induce a wide range of symptoms ranging from allergy-like symptoms to brain fog and can even spiral into the development of serious conditions like kidney damage and cancer
So how is it that some people can come into contact with fungi that are found frequently in the environment and be perfectly fine, while others develop an infection?
What Causes Susceptibility to Fungal Infections?
Anyone can potentially contract a fungal infection, but there are some underlying factors that can make you more susceptible to contracting one such as:6,7
- A weakened immune system that can dampen your ability to combat invading fungi
- An imbalanced microbiome which can allow can allow normally-present fungi to overthrow your beneficial microbes and begin growing out of control
- Excessive or persistent exposure to high levels of potentially harmful fungi (like if you have hidden mold growing in your home)
- An underlying infection that preoccupies and burns out your immune system – allowing opportunistic fungi to invade
- Certain medications that hinder your immune system
- Variations in your genetic coding that can impact how your immune system and microbiome respond to exposure to fungi – making you more vulnerable to fungal infections
With such potentially serious implications, you’re probably wondering what options there are when it comes to treating fungal infections.
Fungal Infection Treatment
Minor fungal infections found on the skin can oftentimes be treated quickly and effectively with topical antifungal creams or ointments. But treating more serious, system-wide fungal infections can be much trickier. You see, there are currently a limited number of antifungal drugs available to treat fungal infections, with the primary classes of antifungal medications being:
- Azole drugs: A class of medications that hinders fungal cells' ability to produce and regenerate their cellular membrane – allowing fungi to be more readily neutralized by your immune system
- Polyene drugs: A class of antifungal drugs that bind to compounds known as sterols found on the outside of fungal cell membranes – subsequently creating pores that impair the integrity of the fungi’s outer membrane
- Echinocandin antifungal drugs: A class of pharmaceuticals that directly inhibits the enzymes that synthesize the primary component of fungal cell walls – compromising their integrity so they can be targeted by your immune system
To further complicate the treatment of fungal infections, many strains of fungi have become resistant to these antifungal medications – rendering the drugs ineffective and incapable of exerting their intended effects. While this resistance to antifungal drugs has left researchers perplexed and frustrated, there is emerging research that might just give us insight into what we can do about it.
The answer to addressing antifungal drug-resistant fungal infections might just lay an essential fungal cell structure known as the mitochondria.
Mitochondrial Function and Fungal Infections
Mitochondria are tiny structures found within the cells of humans, animals, and fungi alike. Mitochondria are considered “the powerhouses” of the cell because they synthesize energy in the form of adenosine triphosphate or ATP via a process known as cellular respiration. But energy production certainly isn’t the only process that these mitochondria play a critical role in.
You see, mitochondrial function plays a pivotal role in fungal virulence and pathogenesis – fungi’s ability to cause disease and how severe the infection is. That’s because mitochondria serve as a sort of central ‘hub’ – coordinating multiple aspects of fungal cell physiology and function such as:8,9
- Iron metabolism and homeostasis: The metal iron is a crucial cofactor or helper molecule in various reactions that are essential for fungal energy production, proliferation, and cell wall integrity.
- Responding to stress: Mitochondria help orchestrate fungal cells' response to stress induced by the host – which in the case of fungal infections would be you and your immune system's response. Stressors might include limited oxygen and/or nutrients, elevated temperatures, pH variability (an acidic or alkaline environment), and chemical or oxidative stress.
- Metabolic flexibility and adaptation: Metabolic flexibility and adaptation refer to the mitochondria's ability to shift the principal types of fuel used to synthesize energy – allowing the fungi to utilize a variety of compounds as a source of fuel or food to survive and proliferate.
- Fungal dormancy: The mitochondria allow fungi to survive in a latent state – essentially laying in wait until your immune system is overwhelmed or compromised. When the fungi sense their window of opportunity, they can then reactivate – proliferating and exerting their harmful effects
So what does this understanding of the role of the mitochondrial mean when it comes to the treatment of fungal infections moving forward?
Fungal Mitochondria: The Key to Addressing Fungal Infections?
Our evolving understanding of the crucial role that the mitochondria play in fungal virulence and pathogenesis gives us promising insight into how we may be able to address antifungal drug resistance. Researchers are hopeful that targeting mitochondrial function may be the key to creating more consistent and effective treatment options when it comes to fungal infections.
While we may have unveiled some exciting and promising discoveries, more time and research are needed to truly determine how these emerging treatment possibilities will unfold. But the good news is, even though we may not have all the answers when it comes to treating fungal infections, there are some steps you can take to help minimize your chances of contracting a fungal infection in the first place.
And the key to accomplishing that is by supporting and enhancing your immune system's ability to defend you against these invading microbes.
How Can I Boost My Immune System Against Fungi?
While we certainly can’t control all of the factors that may contribute to developing a fungal infection – or any disease for that matter – the things we can control can have a monumental impact on our immune system's ability to defend us.
Some simple and potent steps you can take to nourish and boost your immune system include:
- Addressing any underlying fungal infection or fungal overgrowth. Some all-natural supplements that can be helpful in addressing fungal overgrowth and restoring balance are Candida Destroyer and Berberine. Both of these supplements contain compounds proven to have potent antifungal properties.
- Minimizing your exposure to environmental toxins that can bog down and burn out your immune system.
- Detoxing from any accumulated toxins with strategies like PEMF and infrared saunas as well as detox-boosting supplements like N-acetyl cysteine (NAC), Liver Essentials, and ZeoBind Plus.
- Eating a well-rounded, nutrient-dense diet full of a variety of nutritious proteins, antioxidant-rich fruits and veggies, and healthy fats.
- Promoting a healthy gut and diverse microbiome by minimizing gut-irritating foods and adding in gut-supporting supplements like Spore Probiotic plus IgG and Saccharo Force to support a healthy and diverse microbiome full of friendly, health-boosting probiotic bacteria and yeast.
- Incorporating immune boosting supplements like Glutathione Essentials, Immune Essentials, and/or Immune Booster.
- Prioritizing your mental and emotional health by managing stress, spending time with loved ones, and making plenty of time for both fun and relaxation.
- Making sleep a priority. If this one is a struggle for you, you can try all-natural sleep supplements like Dream Powder or Sleep Essentials and try incorporating some of these tried-and-true sleep hacks.
If you’re really ready to dive deeper into some ways to supercharge your immune system, I recommend heading over and reading through the following articles:
- Powerful Ways to Support Your Immune System
- How to Heal Your Gut for a Stronger Immune System
- How to Boost Your Immune System by Reducing Your Toxic Burden
- Vitamin D’s Essential Role in a Healthy Immune System – and How to Get More of It
- How Essential Oils Can Boost Immunity, Alleviate Stress, and Improve Your Health
You can find these articles and many many more over on my blog. And I've got even more helpful, science-backed resources with some of the world’s leading experts over on my YouTube Channel.
Next Steps in Addressing Fungal Infections
Our understanding and ability to treat not only fungal infections, but infections of any kind, is evolving all the time. With each new discovery we uncover, the closer we get to creating effective and lasting solutions. We may not have all the answers yet, but we do have an arsenal of knowledge and tools that can help us bolster our defenses and uplevel our health.
While we certainly can’t control all the factors that contribute to our health and susceptibility to contracting a fungal infection, our day-to-day choices have a monumental impact on our ability to combat and bounce back from any microbes or imbalances that make their way into our lives.
To stay informed and empowered so you can be sure your day-to-choices are supporting vibrant health and longevity without feeling overwhelmed, be sure to sign up for my weekly newsletter by entering your name and email address in the form below. And don’t forget to head over and subscribe to my YouTube Channel.
Now it's time to hear from you. Were you surprised to learn about the incredible role mitochondria play in fungal infections? What are some of your favorite ways to support your immune system? Leave your questions and thoughts in the comments below!
Has there ever been a time in your life when you’ve felt alone or unsure where to turn for answers?
In Unexpected: Finding Resilience through Functional Medicine, Science, and Faith, Dr. Jill Carnahan shares her story of facing life-altering illness, fighting for her health, and overcoming sickness using both science and faith so that others can learn to live their own transformative stories.
Dr. Jill’s riveting and compassionate exploration of healing through functional medicine demonstrates how to replace darkness and fear with hope and find profound healing, unconditional love, and unexpected miracles in the process.
Resources:
- Fungi (Kingdom) – an overview | ScienceDirect Topics
- Fungal Infections | Fungal | CDC
- Types of Fungal Diseases | Fungal Diseases | CDC
- Fungal Infections: Types, Symptoms, and Treatments (healthline.com)
- fe85786a-df67-48de-a60982800c1a0829.pdf (microbiologysociety.org)
- Genetic Susceptibility to Fungal Infections and Links to Human Ancestry – PMC (nih.gov)
- Fungal Infections: Protect Your Health | Fungal Diseases | CDC
- Respiring to infect: Emerging links between mitochondria, the electron transport chain, and fungal pathogenesis | PLOS Pathogens
- System-level impact of mitochondria on fungal virulence: to metabolism and beyond – PMC (nih.gov)
- Are mitochondria the Achilles’ heel of the Kingdom Fungi? – ScienceDirect
* These statements have not been evaluated by the Food and Drug Administration. The product mentioned in this article are not intended to diagnose, treat, cure, or prevent any disease. The information in this article is not intended to replace any recommendations or relationship with your physician. Please review references sited at end of article for scientific support of any claims made.


















Share: