Your immune system is designed to function like a well-trained army – with different molecules, cells, and organs all doing their part to defend you against foreign invaders. And one of the key players tasked with “sounding the alarm” is a little protein known as interleukin-6.
Today we’re going to dive into exactly what interleukin-6 is, what role it plays in inflammation, and how to keep your levels balanced. Let’s dive in.
Exactly What Is Interleukin-6?
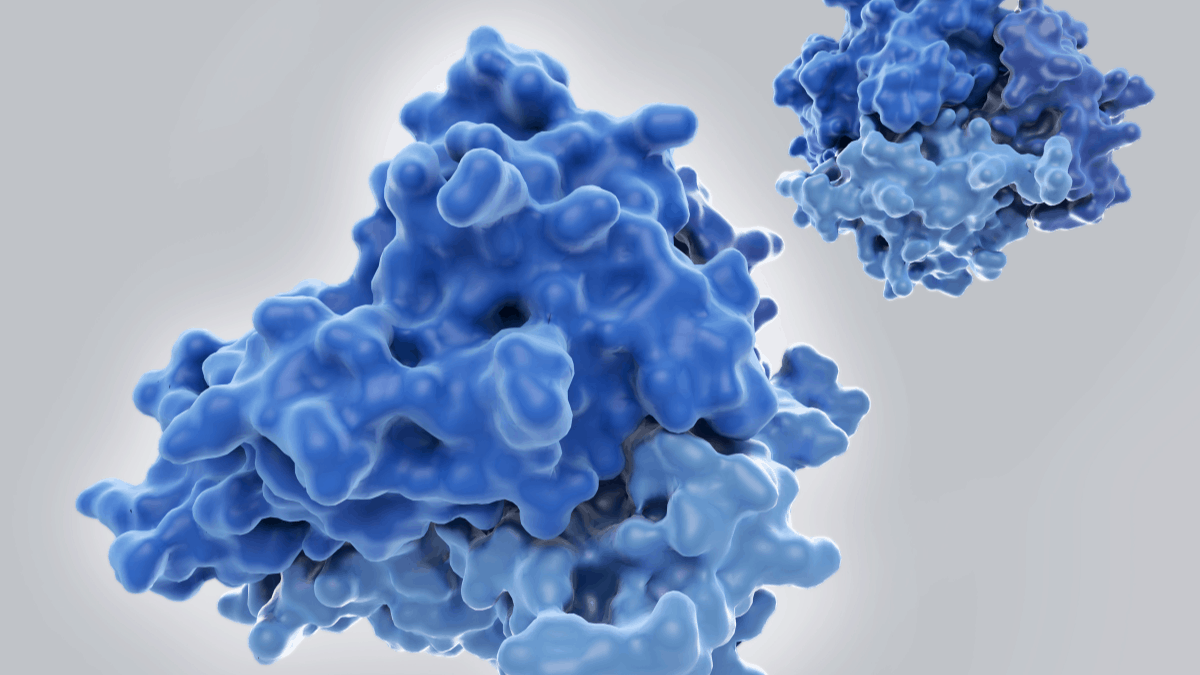
Interleukin-6 (IL-6) is what is known as a cytokine. Cytokines are tiny proteins that act as molecular messengers – allowing cells to communicate with one another by signaling cells to perform certain actions.1
While many cells are capable of producing IL-6, it’s mainly secreted by your white blood cells, also referred to as leukocytes.2 Your white blood cells are key players in your immune response, so their ability to quickly and effectively communicate with the rest of your cells is crucial. You see, your immune system has an army of immune cells that are constantly on watch – scouring your body for anything that might pose a threat.
When your immune cells detect a threat, they “sound the alarm,” flooding your body with chemical messengers like IL-6 that launch your immune system into action in order to neutralize the foreign invader. This activation of the immune system is also referred to as the inflammatory response or inflammation. And IL-6 plays a particularly interesting role in this complex process.
What Is the Role of Interleukin-6 in Inflammation?
When your immune system detects a threat – such as an injury or exposure to foreign microbes – your white blood cells begin releasing IL-6. Once secreted, IL-6 triggers what is known as the inflammatory cascade. The inflammatory cascade is the coordinated and sequential activation of your immune response.
What’s particularly interesting about IL-6, is that it doesn’t just incite the inflammatory response – it also mediates it. What that means is depending on how much IL-6 is released and exactly what cells it targets determines whether it will have a pro-inflammatory effect or an anti-inflammatory effect. So IL-6 can either trigger the immune system to ramp up or down. Some of IL-6’s specific impacts in your immune system include:
- The stimulation of other signaling proteins during the acute phase of inflammation. This release of crucial molecular messengers is pivotal in allowing your body to dispatch an efficient attack against any potential threats.3
- The “capping” of the levels of other cytokines that are pro-inflammatory. IL-6 essentially triggers the “shut off” of pro-inflammatory cytokines, signaling the body to begin resolving acute inflammation and to return to homeostasis.3
- Modulation of the function of macrophages – which are immune cells that are designed to neutralize and engulf any harmful microorganisms so they can be eliminated by the body.4
- The promotion of antibody production. IL-6 encourages immune cells known as B-cells to produce antibody proteins that identify and bind to foreign microbes.5
- The triggering of “sickness behavior” associated with acute inflammation through the activation of the hypothalamic-pituitary-adrenal axis. Sickness behavior includes many of the cardinal side effects of feeling ill such as lack of appetite, lethargy, achiness, and fever.6
Considering that interleukin-6 has both anti-inflammatory as well as pro-inflammatory effects, it raises the question – so is interleukin-6 good or bad?
So, Is Interleukin-6 Good or Bad?
The answer to that question is not so simple. When IL-6 levels are balanced and secreted at appropriate times, this cytokine is more than good – it’s essential. While the term inflammation is often associated with something negative, the inflammatory process is actually important and necessary to keep us alive. Without inflammation, we wouldn’t be able to fight off harmful foreign invaders, heal from injuries, or appropriately respond to potential threats.
IL-6’s role in activating and regulating your immune system is critical. Without IL-6 and other cytokines, we would be vulnerable and unable to defend ourselves. But when IL-6 and other cytokine levels rise too rapidly or remain high for too long, it can spell trouble.
This flooding of cytokines throws the immune system into overdrive and inflammation levels rise. And if levels continue to go unchecked, this inflammation begins causing short-term and long-term damage to your cells and tissues. Over time, this damage accumulates and can lead to a host of problems and diseases.
What Factors Impact Interleukin-6 Levels and Inflammation?
There are numerous factors that influence your IL-6 and cytokine levels, as well as your inflammation levels. And the good news is, you have control over nearly all of these factors. Let's take a look at some of the heavy hitters that have the biggest impact on your immune system and cytokine levels.
Diet
The saying “you are what you eat” couldn't be more true. The foods you consume on a daily basis are the materials and fuel your body uses to function. And the foods you eat either fight inflammation or promote it.
Foods that promote inflammation, dampen your immune system, and contribute to imbalanced cytokine levels include:
- Sugar: This includes not only refined sugar but also simple carbs (like flour) that are quickly converted into sugar by your body.
- Processed foods: This includes nearly anything that is packaged or pre-made.
- Refined oils: Like canola oil, vegetable oil, corn oil, etc.
- Artificial sweeteners: Such as aspartame, sucralose, saccharin, etc.
Foods that fight inflammation are pretty simple to identify. If it’s wholesome, real food, that’s as close to its natural form as possible – then it’s likely anti-inflammatory. To follow an anti-inflammatory diet, I recommend building your meals around foods like:
- Fresh fruits and vegetables: Fresh vegetables and fruits are chock-full of inflammation-fighting antioxidants. Whether you eat them raw or cooked, veggies and fruits are the foundation of an anti-inflammatory diet.
- High-quality protein: Stick to the best quality protein and animal products you can find. I always recommend choosing antibiotic-free, grass-fed, pasture-raised, or wild-caught animal products.
- Healthy fats: Healthy fats that come from whole foods like avocados, nuts, olive oil, etc are also powerful inflammation-fighting foods.
Centering your diet around anti-inflammatory foods doesn’t have to be complicated or boring. Choosing real and whole foods the majority of the time goes a long way in supporting your immune system.
Nutrients
While a healthy diet is the foundation of good nutrition, the truth is, most of us simply can’t get all of our necessary nutrients from diet alone. Thanks to modern agricultural practices and an ever-increasing toxic burden, most of us could benefit from additional nutrients. And supplements are a simple and powerful way to deliver a concentrated dose of nutrients.
When it comes to inflammation-fighting and immune-supporting supplements, these are some of my favorites:
- Mineral Essentials: A combination of essential minerals to fill in any gaps in your diet and replenish your body with all of the vital minerals that support a healthy immune response.
- Probiotics: Your gut and your immune system are intricately linked – without a healthy gut, your immune system cannot function properly. A daily probiotic consistently reintroduces beneficial bacteria and keeps your gut and immune system balanced.
- Vitamin D3: Vitamin D is essential to proper immune function and keeping inflammation levels in check. In fact, a deficiency in Vitamin D has been directly linked to a weaker and less effective immune response.
- Vitamin C: Vitamin C is a potent antioxidant that fights the oxidative damage caused by harmful free radicals associated with inflammation.
If you’re interested in learning more about exactly how supplements can give your immune system a boost, I recommend heading over and reading my article all about the Best Immune Boosting Supplements.
Sleep
Sleep deprivation is like kryptonite to your immune system – causing inflammation levels to spike and throwing your entire system out of whack. So prioritizing sleep is crucial when it comes to your immune health and keeping inflammation at bay.
When it comes to sleep, you want to focus on both quantity and quality. Ideally, you want to log 7-8 hours of sleep each night. And when it comes to quality, you want uninterrupted and restful sleep. Sometimes getting quality sleep is easier said than done, so some simple steps that might help improve your sleep quality include:
- Keep your room cool, dark, and comfortable
- Block out any sounds that might disturb you by using a fan or white noise
- Shut off all electronics at least 30 minutes before bed
- Establish a nighttime routine that eases your body into a relaxed state
If you have trouble falling or staying asleep, an all-natural sleep aid like LipoCalm might help.
Taking a Big Picture Approach to Inflammation and Health
Your immune system and your body’s inflammatory response are complicated. Understanding the role IL-6 and other cytokines play in inflammation is important, but the truth is, it’s really just a small piece of the puzzle.
When it comes to keeping inflammation levels in check and keeping your immune system firing on all cylinders, we have to take a big picture approach. There’s no single factor that’s going to optimize your health and bolster your defenses. The lifestyle choices you make on a daily basis are what truly impacts your health and well-being. And it’s my mission to bring you the resources and knowledge you need to make healthy lifestyle choices easier to incorporate into your daily life.
If you enjoyed this article and are interested in learning more about how you can advocate for you and your family’s health and well being, I’ve got tons of resources on my blog – you can check it out by clicking here. And if you want to take it even deeper, I encourage you to sign up for my newsletter. You’ll get my very best advice and resources delivered straight to your inbox. All you have to do is enter your name and email address in the form below.
Now it’s time to hear from you. Were you surprised to learn that interleukin-6 is both pro-inflammatory and anti-inflammatory? What steps are you taking to keep your inflammation levels in check and support a healthy immune system? Leave your questions and thoughts in the comments below!
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2785020/
- https://www.cancer.gov/publications/dictionaries/cancer-terms/def/interleukin-6
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3226076/
- https://www.frontiersin.org/articles/10.3389/fmicb.2019.01057/full
- https://www.hindawi.com/journals/ijr/2011/721608/
* These statements have not been evaluated by the Food and Drug Administration. The product mentioned in this article are not intended to diagnose, treat, cure, or prevent any disease. The information in this article is not intended to replace any recommendations or relationship with your physician. Please review references sited at end of article for scientific support of any claims made.


















5 Comments
Hubby’s inflammation is off the charts He has stage 4 CKD and an extremely inflamed bladder( they took biopsies for cancer).He is on Sodium Bicarbonate…4 capsules a day..each one 650 mg.He also takes 1, 2000 iu vitamin D3 and a 750 mg Curcumin( turmeric) supplement. My poor husband seems to be in some sort of cytokine storm!! 😕
Hi Charlene
I am so sorry to hear it! Once the immune system gets aggravated it can be hard to calm the inflammatory cascade of cytokines.
Warmly,
Dr. Jill
THANK YOU for sharing your wealth of information!
As a Functional Nutritionist, I lecture educating individuals the importance of BRAIN/GUT health along with triggers in our Environment which can lead to autoimmune illness. I am currently going through the FNLP program through Functional Nutrition Lab and enjoying connecting with like-minded people!
Dear Dr Carnahan,
What test(s) do we ask our doctors to run to check for IL-6 inflammation? Seems like the allopathic doctors just run the standard CBC blood test, and if they talk about inflammation, they don’t do any tests. They just prescribe an NSAID.
Many thanks for the great information.
Share: