Our immune system is a powerful force inside each one of us! This protective system is charged with the job of responding to foreign invaders to keep us in optimal health. Most of us don't think too much about this system until it is not working correctly. I treat many patients that suffer from overactive or under-active immune systems due to chronic infections, like tick-borne diseases; toxic exposures, like mold and mycotoxins; or autoimmune diseases, like multiple sclerosis, lupus or Hashimoto's thyroiditis. Although many patients understand the important role of the immune system in protection and defense, few people know that it also controls our behavior. A recent study in Nature discussed the role of cytokines activated when the immune system goes on red alert and the connection to social isolation and autistic behaviors. It's even plausible that changes in immune function may lead to personality changes!
Interferon-Gamma: a Key Immune Signal
One of the key molecules is interferon-gamma (IFN-gamma) secreted by activated white blood cells of the immune system. Once this molecule crosses into the brian it inhibits the neurons in the pre-frontal cortex. If the pre-frontal cortex is inhibited, the patient actually becomes more social. So if the immune system is activated, a person may feel more social. However, in a patient with an immune deficiency we may see the opposite effect, more isolation and antisocial behavior. This new data suggests that an impaired immune system may contribute to numerous neuropsychiatric conditions. It may contribute to isolation or depression when someone is sick and the immune system is not functioning properly. As we learn more it may help us to understand the difficulties faced by those with immune dysfunction due to chronic infection or toxic mold exposure. It may even lead to changes in the relationships to people closest to us, such as our friends, children and spouse if they do not understand the effect of the illness on your decreased desire for social interactions.
Inflammatory Cytokines and the Brain
A recent article about inflammatory cytokines and brain signaling discussed inflammation and the brain:
When considering the pathological signaling cascades in immunological disorders of the brain, certain cytokines might be considered of key importance, with their presence determining the course of a particular disease. Interleukin-1 (IL-1), IL-6, IL-17, and TNFα are critical for the pathogenesis of inflammation in certain brain disorders. Targeting these cytokines or their receptors can alter the course of several neurological diseases, but the effects may be beneficial or harmful.
We understand from this article that the inflammatory signals of the immune system (cytokines) have a profound effect on the brain. Many patients battling systemic inflammatory or autoimmune disorders suffer from an “inflamed brain” and all that goes with it… symptoms like depression, anxiety and insomnia. The role of cytokines on behavior can be summarized by saying that TNFα (sickness and depression) and IL-1β (sickness) alter behavior by direct actions on neurons of the brain.
Gaba may affect the immune system too…
GABA, an inhibitory neurotransmitter in the brain, has a similar inhibitory effect on the immune system. Antigen presenting cells (APCs) of the immune system have gaba receptors and therefore, gaba can directly inhibit the function of these immune cells. What this means is this neurotransmitter from the brain may have a direct inhibitory effect on the body's immune system. This article on Gaba and the immune system states….
Intricate and reciprocal regulatory relationships exist between the nervous system and the immune system, mediated in part by chemical messengers, like Gaba. This has been clearly demonstrated for the central nervous system through the hypothalamic–pituitary–adrenal axis.
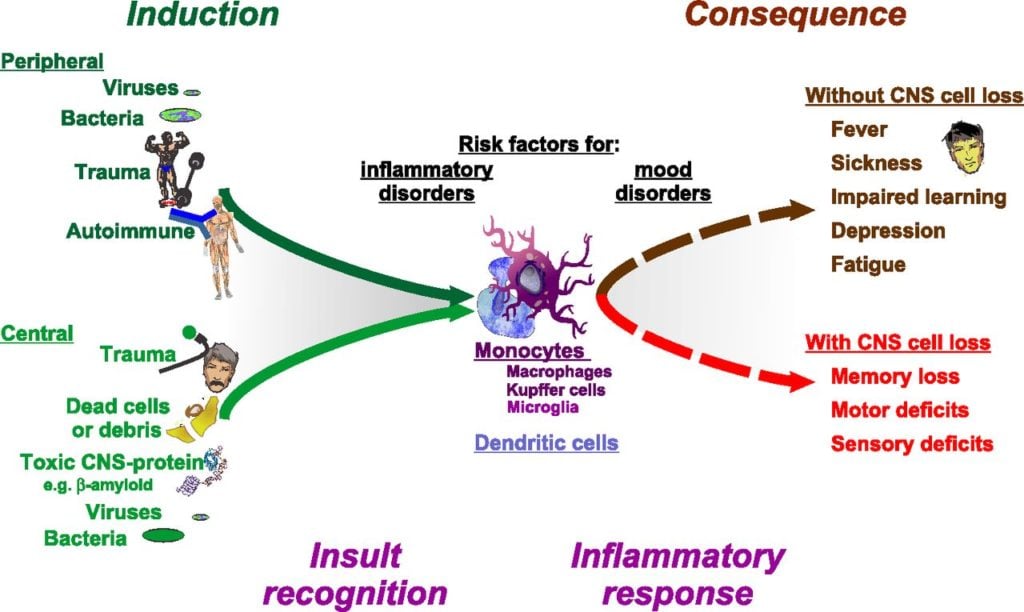
Insults to the body, from the outside or from the inside, activate cells of the innate immune system. The immune response transmits this information to the brain to cause physiological and behavioral responses. A mild inflammatory response – such as a low-grade infection, trauma (such as dropping a weight on one’s foot) or even strenuous exercise – results in reversible consequences as they are a result of altered cellular (neuron) function. A severe response induces often irreversible consequences as a result of cell death. In either case, the causal event is initiated by monocytic and dendritic cells with the initiation of an inflammatory response.
[PHOTO SOURCE HERE]
Sickness and Depression
Perhaps no connection has been more studied than that of immune activation and inflammation and the link to depression. Systemic infections cause the patient to allocate limited resources, conserve energy and prevent spread of infection. The resulting sickness behavior is common to most infections, including viruses, bacteria and multi-cellular parasitic infections. There is a broad spectrum of symptoms – fever, nausea, decreased appetite, malaise, fatigue and achiness – all of which may aid in the fight to conserve resources and increase isolation-type behavior. In animal models we see sickness associated with a decrease in time seeking interaction with a other animals as a result of diminished motivation for social exploration. Symptoms of depression appear after pro-inflammatory cytokines are produced by the body or if they are administered experimentally. The fact that inflammation often leads to later depression suggests a cause–effect relationship. It indicates that immune activation can precipitate depression. Many symptoms of inflammation-induced depression overlap with sickness behaviors, including fatigue, changes in sleep pattern, lack of interest in daily or pleasurable activities (anhedonia), changes in appetite or body mass and unexplained aches and pains
The Journal of Experimental Biology Article concludes:
(1) Independent of the type of infection, the inflammatory response may cause behavioral changes.
(2) Pro-inflammatory cytokine expression is a precursor for behavioral changes.
(3) Behavior is controlled by neuronal function. Behavioral changes associated with infection are a result of inflammatory cytokine interaction with neurons.
So perhaps we should dig deeper if we or a loved one is experiencing depression and finding less pleasure in social activities. It is quite possible that hidden infection or an inflammatory condition may be the cause of the personality changes. Bottom line is have compassion… there is more to it than meets the eye!
* These statements have not been evaluated by the Food and Drug Administration. The product mentioned in this article are not intended to diagnose, treat, cure, or prevent any disease. The information in this article is not intended to replace any recommendations or relationship with your physician. Please review references sited at end of article for scientific support of any claims made.



















15 Comments
Oh my goodness. Thank you for this insightful look into the immune system and our behaviour. It just so happens that since moving into our home when our son was 4 weeks old, my immune system took a major dive for the worse and our son too has never been well, whilst living here. It turns out that within a year of moving into this home, I was diagnosed with Hashimotos thyroiditis and after being medicated for 4 years, decided to try to find some answers for myself and discovered I had mould and suspect our now 5 year old also has mould. His behaviour has really chanced since toddlerhood from a happy go lucky child to a rather morose, defiant, bordering on schizophrenic like behaviours at times. I have had a gut feeling that it wasn’t him per say and more of a biological/environmental influence. This article certainly leads me to think I might be on the right track with my suspicions. Sadly there doesn’t seem to be a medical empathy or even understanding that this could be so, so I imagine in the next few years as he starts school, we will have paediatricians wanting to medicate him for ADHD and ODD! I will, of course, be very resistant to this kind of bandaid treatment.
Thank you again for your research. I wish you could study my son as we are about to move out of this home to hopefully a lot cleaner environment where I will use binders on both my son and I to try to rid our bodies of this horrid mould.
Thank you so much for all your work in this area. This makes perfect sense. I have been sick mostly my whole life. Both my adult daughters also have chronic health problems like myself. My oldest was diagnosed with fibromyalgia at age 12 and my youngest was born with group be strep that led to sepsis and airlifted to Duke Hospital in Durham , NC where she was placed on a life support machine called ECMO. She developed 2 grade 4 bleeds immediately but had to stay on the machine 9 days to save her life.
My health was poor before I married but after marrying my wonderful husband we moved into his grandparents home that was built in 1902. Immediately I began to have severe fatigue, physical pain and digestive issues. Our oldest daughter was 2 when we moved into the home and prior to this she was a very healthy girl except having severe eczema and learned she was allergic to cigerette smoke . ( she and I lived with my parents before I married my husband for 2 years and they were heavy chain smokers.)
We moved from our old home September 24, 2015. Prior to moving I had our well water tested because I had always felt the water was what made me and both my daughters sick. My husband was a firefighter and was gone for 24 hours every 48 and worked a second job, he experienced increase fatigue but was gone more from the home and I think that is one reason he never developed the health problems me and the girls did. When I called the county we lived in to ask someone to test our water ( we had a filter system put in about 20 years after moving in, it was in the basement .) Whrn I called the county to come out and test our water, I was told for the first time we lived in a hug risk zone. ( I had called the county several years back to ask had there been any reports of health concerns in our area because there was a lot of cancer on our dead end street, every home had cancer at some point and this was an old established neighborhood, my husbands old stomping grounds as a kid and most everyone still lived on the street including his parents and uncle that lived on each side of our home .)
The county told me the first time I called there were no reports filed or concerns. But when we had the water tested straight from our well and 5 other neighbors water tested from their wells, we learned that the old gas station right across the street did not remove their old gas tanks until 1995. This was 12 years after we moved into our home, after my husbands mother died from cancer, our neighbors mother died from cancer, my husbands aunt had breast cancer twice and just numerous health issues throughout this small dead end street across from this old gas station.
I feel that is where my health truly began to decline and why both my girls have had many health problems.
We have no moved to Mebane, NC and that was to get away from the home itself and to get closer to Duke. My youngest has been a patient there since being airlifted 25 years ago. Her brain injury has truly impacted her in many ways. My oldest is not much better. She is anemic and has a high protein level we have been told is due to inflammation. My digestive system is failing amongst other things. Waiting to be seen by a genetics specialist to be tested for Mast Cell Activation Disorder. I have learned a lot about medical conditions because my girls being so sick and myself, I have always known there was an environmental connection. Now, just trying to find the right doctor that will work with me to put the puzzle together as opposed to being overwhelmed by our long list of health problems. Fortunately we have some amazing doctor’s at Duke that have taken good care of my youngest. Now to get me and oldest established.
Not sure if a genetics specialist is the right direction but the new NP I am seeing was very overwhelmed by my illnesses and truly did not want to discuss any of them except 1 thing that was bothering me as opposed to helping me piece it together. She is the one sending me to a genetics specialist , even though I asked to see an immunologist. I had to give her a reason for wanting to see an immunologist so she wrote down Mast Cell Activatin Disorder has a possible diagnoses, at my request.
I had shared a bit with you awhile back and you suggested I see a specific doctor. If you could tell me once again the right doctor to see as far as looking at environment affects and defiantly inflammation issues with me and my girls.
I really needed to read this today. My decrease in health has truly affected my brain. Misdiagnosed with mood disorders and was on tons of f medication many years ago that I slowly weaned myself off of and it was like the lights came back on in my mad, felt so much better. But the chronic pain and inflammation I am having daily is taking a tremendous toll of my m d and emotions. It has also done the same with my girls.
Thank you for looking outside the medical box so many doctor’s tend to stay in when a Zebra walks in their office.
God Bless you and keep teaching the medical community and folks like us.
Hi Sheila
I suggest finding a functional medicine trained doctor in your area. You can search by zip code at http://www.functionalmedicine.com. Have you read my article on Health effects of mold exposure?
warmly
Dr Jill
Hi Sheila, if you are close enough to Charleston SC I suggest going to the Center for Occupational and Environmental Medicine. They have 50 yea s of dealing with mold and other toxic elements. I personally see Dr. Herbert who is IFM certified as well as several others.
Thank you for this article. I am 26. I got very ill after being exposed to toxic black mold. My fiance and son got respiratory issues while my symptoms were all neurological. First was confusion and heavy brain fog than fatigue, than the worst of all symptoms together was the Anhedonia. Feeling very disconnected to my surrounding but still in my body. I have no history of mental illness nor does it run in my family. As I complained to my primary of my symptoms I was sent to the mental health department after the CT scan it begged her to order and CBC and hormonal panel came out normal. I went on ssri to MAOI with no relief. I would cry everyday because I would hold my 1yr old child and feel nothing. My life was 100% pleasureless, no mental clarity and I wanted to die. I went on to try Ketamine in LA. Did nothing and TMS for 6 weeks with no lift in my Depressive state and fatigue. I lost all hope.
Although I left my original place where I got exposed, all my symptoms were still present. I put the connection together after reading articles on inflammation and treatment resistant depression. I was barely functional but was desperate to get my life back and ran across survingmold. com and I found my answer after seeing over 20 doctors. Now on VIP for almost a week and I plan on camping outside while I am on my protocol. I hope to feel some progress. This article can save someone’s life who has an on set of Depressive symptoms with no explanation. Thank you for bringing awareness. I know there are many other suffers who are going through my struggle and I hope they can find their way to this well written article and seek a physician that wont think they are crazy for suggesting Mold may have caused their psychological issues and cognitive decline. The kind of depression inflammation of the brain can bring on is painful beyond imaginable and although I still suffer from complete Anhedonia which I hope it goes away with treatment, I am grateful this topic is getting more light. Thank you
Very nice article. So if one has the symptoms caused by increased cytokines, how does one reverse it?
Hi Tim,
Find the root cause… infection, stress, toxin, nutritional imbalance, etc and treat that
warmly
Dr Jill
Hi Dr Jill, My 15 yr old son has had SIBO and bartonella for the past year. currently doing second treatment for both. Have used Rifaxamin , Naltrexone, Low Fodmap diet since 12/15. He is still producing methane and fluctuates between consitpation and diarraeah . Currently, using Rifampin, Metrodiazonole and Naltrexone along with SCD and Lowfodmap diet. Upper Endoscopy revealed moderate GERD damage to Esohpogus due to overproduction of acid. which is being addressed with HCL/betaine and ginger tea. Also did a month of Naturethroid to see if this would cause his bowels to function normally, It was not a good response as he was dizzy and lightheaded during the entire 30 day course. So functional med doc took him off and started him on this new regimen. Rifampin He was so impacted all the way to the ascending colon, until 13 colonics were performed to eliminate old stool. SOn had constipation and bedwetting issues since potty traiing in addition to major learning issues and brain fog . The underlying casue was never identified. Would a colonoscopy assist at this time to determine any underlying cause of his current symptoms- fatigue, muscle aches, sense of fullness after eating and at night while sleeeping.’
so what is left to do prevent relapsing. Colonoscopy more bloodwork or gastro. Your input would be much appreciated
thanks much blessings pam
Hi Pamela,
When there is autonomic dysfunction due to tick-borne illness, SIBO may be persistent and difficult to eradicate.
warmly
Dr. Jill
Dr c, thanks so much for your response . Do colonoscopies offer any insight into causal relationship to chronic constipation , bloating and diarrhea once SIBO is diagnosed , we actually had a clean SIBO test once we treated 2 time , but gas and bloating led dr to retreat SIBO with ridampin and metrodiazonole
Colonoscopy will rule out other more serious issue such as stricture and cancer.
Hi just curious, what would cause a severe response cause irreversible damage to neurons. I had s big exposure cause heavy neurological issues and as well as the the sickness behaviour you mentioned. I havent been in treated for about a year and a half due to to bring misdiagnosed. It is possible that this is too late to be reversed? I have bad anhedonia, fatigue and horrible cognitive issues. I was exposed to high amounts of mold and that’s how I sick. And have been exposed since. I’m going to start treatment soon. Thank you
Immune inflammation and autoimmunity may cause severe neuroinflammation
Share: