Cancer. A word that everyone knows but no one is ready to hear.
This devastating disease has touched countless lives worldwide and has long been the subject of intensive research and treatment efforts. As our understanding of this complex disease evolves and we continue to race to find a viable cure, researchers are now turning their attention to a new player in the fight against cancer – the invisible universe of microbes teeming within us known as our gut microbiome.
Today, we’re going to explore the fascinating and potentially promising link between the gut microbiome and cancer. Let’s start by zooming in on what cancer is and how your cells become cancerous in the first place.
Cancer Explained: How Does Cancer Start?
Cancer is a complex group of diseases in which some of your body's cells grow and divide uncontrollably. You see, normally, your cells grow, divide, and die in a controlled manner – forming new cells to replace old or damaged ones. This process of normal cell growth and division is tightly regulated by various signaling pathways and checkpoints in the cell cycle.
But cancer cells defy this normal regulation. And once these regulatory mechanisms become disrupted or damaged, your cells can start to grow and divide abnormally and at a rapid pace – leading to cancer development. There are numerous factors that can come together to spark this transformation of normal cells into cancerous cells which can include:1,2,3,4
- Genetic mutations: Your genes are like the instruction manual that tells your cells how to function, grow, and divide. Changes or mutations in the DNA of cells can disrupt their normal function and lead to uncontrolled growth.
- Epigenetic changes: Gene expression is the process that determines whether a gene is “turned on” or “turned off” within a cell. Epigenetic modifications can alter gene expression without changing the DNA sequence. Changes to how genes are expressed can play a pivotal role in whether or not cells become cancerous.
- Chronic inflammation: Inflammation is a healthy and crucial process designed to ramp up for a short period of time, and then ramp back down to baseline. But ongoing, long-term inflammation can create an environment that promotes cell damage and genetic mutations – increasing the risk of cancer.
- Carcinogens and environmental toxins: Carcinogens (substances known to cause cancer) and other toxic compounds that we encounter in our daily lives can trigger inflammation, mimic hormones, and impair detoxification – all of which can spur the changes that trigger cancer development.
- Immune system dysfunction: A healthy immune system can detect and eliminate cancerous cells. But sometimes, your immune system can malfunction – allowing cancerous cells to evade the immune system's surveillance.
There are countless genetic, environmental, and lifestyle factors that can contribute to these underlying changes in the body that can set the stage for cells to become cancerous. But what happens once cancer has set in? Is it possible to cure or treat these malfunctioning cells?
Can Cancer Be Cured Or Treated?
The term “cure” in the context of cancer can be complex. In some cases, cancer can be put into remission – meaning all signs of cancer are eliminated. Other times, the goal of treatment is to control the disease, slow its progression, and manage symptoms to improve your overall well-being. And unfortunately, in some cases, treatment is aimed at simply relieving symptoms, improving the quality of life, and managing side effects when remission is no longer possible.
Traditional cancer treatment can entail a variety of different approaches including:5,6
- Surgery: The surgical removal of tumors and any cancerous growths.
- Radiation therapy: The use of high-energy radiation to target and destroy cancer cells or to stop their growth and division.
- Chemotherapy: The use of powerful drugs to kill or slow down the growth of rapidly dividing cancer cells in the body.
- Immunotherapy: A treatment that boosts the body's own immune system to recognize and attack cancer cells more effectively.
- Targeted therapy: The use of drugs or other substances to specifically target and block the growth and spread of cancer cells, while causing less damage to normal cells.
While radiation, chemo, and other cancer-targeting therapies can certainly be life-saving and dramatically increase your chances of surviving and beating cancer, it is crucial to also incorporate specific lifestyle changes. Creating an “anti-cancer” lifestyle encompasses a variety of lifestyle factors ranging from your diet to your sleep and from your toxin exposure to your stress levels. And one lifestyle change in particular that has been found to have a potentially significant impact on cancer, is the health of your gut microbiome.
What Is Your Gut Microbiome?
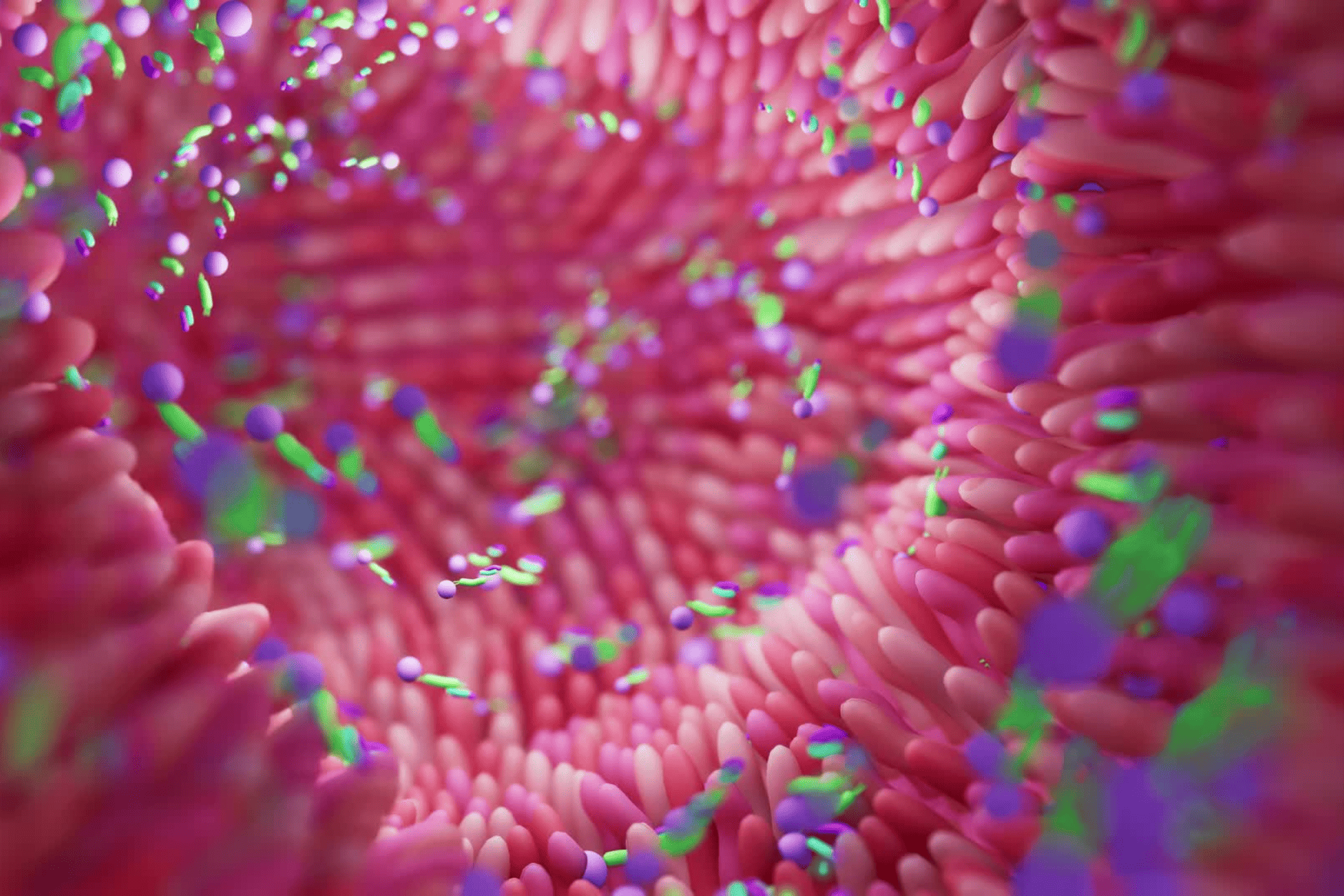
Your gut microbiome refers to the complex community of microorganisms that reside in your digestive tract – primarily in your large intestine. It is composed of trillions of microbes, including bacteria, viruses, fungi, and other microorganisms – all of which are designed to work in harmony with your own cells to maintain just about every aspect of your health and well-being.7
Each person's gut microbiome is unique and influenced by various factors, including genetics, diet, lifestyle, environment, and early-life exposures. But one thing that all of our gut microbiomes have in common, is that they are meant to operate as an interconnected ecosystem full of a diverse variety of different and distinct microbes.
If this fragile ecosystem gets thrown out of whack, it can have a massive impact on your health and contribute to the development and progression of countless conditions – including cancer.
Your Gut Microbiome and Cancer: How the Microbiome Affects Cancer
Research is finding that your gut microbiome can potentially impact not only the development of cancer, but also how your body responds to cancer treatment, and your chances of both survival and remission. It’s speculated that your gut microbiome can influence cancer in the following ways:8,9,10,11,12
- Inflammation modulation: Your microbiome can either support or combat inflammation. An imbalance in your microbiome or an overgrowth of certain gut microbes can promote inflammation – creating an environment that fosters the growth of cancer cells and supports the formation of tumors.
- Immune system regulation: Your gut microbiome plays a crucial role in how your immune system responds to potential threats. It accomplishes this by modulating immune cells' function and activity while influencing how your immune system recognizes and responds to cancer cells.
- Production of metabolites: The microbes in your gut break down the food you ingest and produce by-products or metabolites such as short-chain fatty acids (SCFAs), trimethylamine n-oxide (TMAO), conjugated linoleic acid (CLA), and others. These metabolites can have potent anti-cancer effects by directly influencing cancer cells' behavior, affecting tumor growth, and altering signaling pathways as well as the surrounding microenvironment.
- Modulation of hormones: Certain gut microbes can metabolize hormones, including estrogens, which may have implications for hormone-related cancers such as breast cancer.
- Activation or detoxification of carcinogens: Some gut microbes can enhance the metabolism and detoxification of carcinogenic toxins. And others can increase the activation of these pro-carcinogenic compounds.
- Gut barrier integrity: Your gut barrier is designed to stay sealed up tight – locking toxins, harmful pathogens, and waste materials in your intestines to be eliminated. An imbalanced microbiome can disrupt the integrity of this barrier – allowing harmful substances to enter your bloodstream and potentially contribute to cancer development.
- Anti-tumor immunity: Your gut microbiome can influence the effectiveness of anti-cancer immune responses – with certain gut microbes enhancing the activation of immune cells that target and eliminate cancer cells.
- Drug metabolism and efficacy: The microorganisms that reside in your gut can influence the metabolism and effectiveness of certain cancer drugs which can have a dramatic impact on outcomes as well as side effects.
- Gut-brain axis: Your gut microbiome communicates directly with your brain via the gut-brain axis – influencing stress responses and neural pathways related to cancer development and progression.
The discovery of just how powerful the microbiome can be when it comes to cancer is promising and exciting. And while the microbiome isn’t necessarily the end-all-be-all of curing cancer, it can certainly give us an edge in preventing and fighting back against cancer. So how can you best create and support a flourishing and diverse gut microbiome?
How Can I Restore My Gut Microbiome Naturally?
Creating a lifestyle that supports a thriving and balanced microbiome is hands down one of the most critical things you can do for your overall health and can be especially important if you’ve had any history with cancer. Here’s what I recommend to restore and support a happy healthy gut:
- Eat a diverse, anti-inflammatory diet: Your diet is the foundation of your gut health. Try building the majority of your meals around organic, whole foods as close to their natural form as possible. And limit your intake of processed, sugar-laden food. If you need some ideas to spice it up in this department, be sure to check out my recipe library.
- Consume foods that are rich in prebiotics and probiotics: Probiotics are friendly bacteria that support your gut and prebiotics are the types of fiber that these microbes use for fuel. Try incorporating probiotic-rich fermented foods like yogurt, kefir, sauerkraut, kimchi, and miso as well as prebiotic-rich foods like onions, garlic, leeks, asparagus, bananas, and chicory root, to nourish and stimulate the growth of beneficial gut bacteria.
- Avoid unnecessary antibiotics and antibacterial products: Antibiotics certainly have a time and place, but they can decimate your gut microbes by killing both harmful and beneficial bacteria. Excessive use of antibacterial products (like soaps and cleaning products) can also interfere with the natural balance of gut bacteria.
- Don’t underestimate the power of rest and relaxation: Sleep deprivation and chronic stress can negatively alter the composition of your gut microbiome. Make sure you’re logging plenty of quality sleep and try incorporating stress-reducing techniques like meditation, yoga, deep breathing, or spending time in nature.
- Get moving: Regular exercise has been linked to a more diverse and beneficial gut microbiome – so find some form of movement you enjoy and commit to at least a few minutes each day.
- Reinoculate your gut with probiotics: It can be immensely helpful to reintroduce beneficial bacteria into your gut by taking a daily probiotic supplement. Because diversity is key when it comes to your microbiome, I recommend taking both traditional Probiotic Essentials alongside Spore-Based Probiotics. It can also be helpful to ensure these microbes have plenty of fuel by adding in Prebiotics too.
- Bolster your gut lining with gut-supporting nutrients: Your gut requires plenty of raw materials to build and maintain a strong barrier. Incorporating nutrients like Gut Shield, Collagen, and Gut Calm can ensure you have a well-fortified gut.
- Minimize exposure to environmental toxins: Toxins can be lurking everywhere in our day-to-day lives. Limit the amount of toxins sneaking their way into your body by filtering your air, purifying your water, and making low-tox swaps.
If you are currently in the trenches battling cancer or working hard to keep cancer in remission, I strongly encourage you to consider working with an experienced Integrative and Functional Medicine Doctor to help you not only maximize the health of your gut microbiome but help you create an anti-cancer lifestyle. They can help you take the guesswork out of what steps to take next and work in conjunction with your oncologist and other doctors to help you fight back against cancer.
So, Can Your Microbiome Really Increase Your Chances of Beating Cancer?
The answer to that question is – it’s complicated. There’s no cure for cancer and there is no solitary lifestyle change that’s going to single-handedly turn the tide when it comes to cancer. While there are no guarantees, there are things you can do to support your body and help stack the deck in your favor. And supporting a healthy, diverse gut microbiome is one of those things.
Again, if you’ve had any brush with cancer, I cannot overemphasize the importance of seeking out the guidance of an experienced Integrative and Functional Medicine Doctor to help create a path for healing that’s as unique as you are. And I strongly encourage you to continue educating yourself and arming yourself with as much knowledge as possible so you can make informed and empowered choices about your health.
That’s why I’m so dedicated to providing science-backed and easy-to-understand information on my blog and my YouTube channel – to provide my patients and readers with tools to empower themselves. But sometimes, we all need more than just facts and knowledge – sometimes we simply need to know that we’re not alone and that there is hope for a brighter future. And that is exactly why I wrote my book Unexpected: Finding Resilience Through Functional Medicine, Science, and Faith– to help inspire you to keep overcoming even in the darkest of times.
Now it’s time to hear from you. Were you surprised to learn just how big of an impact your gut microbiome can have when it comes to cancer? Do you have any gut-supporting tips to add to the list? Leave your questions and thoughts in the comments below!
Resources:
- What Is Cancer? – NCI
- Epigenetic Determinants of Cancer – PMC (nih.gov)
- Inflammation and Cancer – PMC (nih.gov)
- atsdr.cdc.gov/emes/public/docs/Chemicals, Cancer, and You FS.pdf
- Treatment for Cancer – NCI
- Cancer treatments: MedlinePlus Medical Encyclopedia
- Part 1: The Human Gut Microbiome in Health and Disease – PMC (nih.gov)
- Analysis of the fecal metagenome in long‐term survivors of pancreas cancer – Kharofa – 2023 – Cancer – Wiley Online Library
- Frontiers | New Insights Into the Cancer–Microbiome–Immune Axis: Decrypting a Decade of Discoveries (frontiersin.org)
- The microbiome and human cancer – PMC (nih.gov)
- Emerging role of human microbiome in cancer development and response to therapy: special focus on intestinal microflora | Journal of Translational Medicine | Full Text (biomedcentral.com)
- The role of gut microbiota in cancer treatment: friend or foe? | Gut (bmj.com)
* These statements have not been evaluated by the Food and Drug Administration. The product mentioned in this article are not intended to diagnose, treat, cure, or prevent any disease. The information in this article is not intended to replace any recommendations or relationship with your physician. Please review references sited at end of article for scientific support of any claims made.


















Share: