In one way or another, we’re all touched by depression. But if you or a loved one has ever sought help for depression, you’ve probably come across the same textbook explanation: Depression is a result of chemical imbalances in your brain that affect your mood.
In other words, depression is “in your head.”
At one point in your research, you may be wondering: How do psychiatrists know that your brain chemicals are out of whack?
The truth is they don’t.
And while we’ve certainly come a long way in speaking more openly about depression and other mental health disorders, we still understand very little about the physiological factors and processes that contribute to depression.
But recent research indicates there is a new (yet unsurprising) culprit in town: Inflammation.
Some have suspected it for decades, but new scientific evidence clearly shows that inflammation plays a huge role in depression.
Unraveling the Mind-Body Connection
For centuries, western medicine has been based on the philosophical tradition of dualisms and dichotomies. Where the mind and the body exist as two separate entities with a vague point of connection between them. In other words, we tend to separate systems in the body.
However, researchers in philosophy, cognitive science, and psychology have challenged this standard, advocating instead for an “embodied cognition.” This is the idea that the mind is not only connected to the body but that the body and its experiences influence the mind – and vice versa. Despite research that supports this concept, healthcare professionals have yet to reach a consensus. And so the field of psychology is characterized by polarized schools of thought.
Let’s look at an example.
You probably already know that many types of arthritis – rheumatoid, psoriatic, and ankylosing spondylitis among others – are caused by inflammation. But in many patients, joint pain is not the only symptom they suffer from. People with arthritis often experience:
- Low energy
- Prolonged periods of sadness
- Hopelessness
- Worthlessness
- Sleep disturbances
- Guilty thoughts
All of the above are also classic signs of depression.
Now, you may be thinking, “Of course they are depressed! Wouldn’t you be if you were in that much pain?”
This is a dualist medical explanation. The body is in pain from arthritis, which can be explained by inflammation. The changes in mood and behavior are explained by the patient thinking about the implications of having arthritis. Simply put, they suggest the state of the mind reflects the physical state, not that the inflammation of the body affects changes in the mind.
But the embodied cognition approach provides a new, simpler logical explanation: A person with arthritis is not depressed because they think about being inflamed and in pain, but they are depressed because they are inflamed.
To accept this new way of thought, scientists had to answer one big question: How do the inflammatory changes in the body cause changes in the brain to make people depressed?
Thanks to new research, scientists have identified a few mechanisms through which inflammation can cause depression.
Inflammation is a Major Driver Depression
Scientists once believed that the immune system was kept separate from the brain by the blood-brain barrier (BBB). The blood-brain barrier is a microvasculature system that regulates the movement of substances like cells and proteins between the blood and the central nervous system.
Essentially, the blood-brain barrier was the physical representation that supported the ideas of a mind-body dichotomy or separation. After all, how could important proteins in the blood affect the brain if they couldn’t cross the blood-brain barrier?
But researchers now know that there are certain types of proteins that can cross the blood-brain barrier. In particular, there is one category of proteins with this ability that can create powerful inflammatory effects throughout the entire body, including the brain.
These inflammatory proteins are called cytokines.
What Are Cytokines?
Cytokines are messenger molecules responsible for regulating cell-to-cell interactions and communications. They are powerful regulators of the immune system’s inflammatory response to disease and infection, as well as normal cellular processes.
Although the term cytokines refer to a large group of proteins, they can be divided into two groups based on their functions:
- Pro-inflammatory
- Anti-inflammatory.
A subtype of white blood cells called T lymphocytes are a major source of cytokines. T lymphocytes are an essential part of your immune system. They recognize foreign particles with their highly variable cell-surface receptors. Of the various types of T lymphocytes, T cells are known as the predominant producers of cytokines. T cells can be further divided into two groups:
- T helper (Th) type 1
- T helper (Th) type 2
Pro-Inflammatory vs. Anti-Inflammatory Cytokines
Cytokines secreted by Th1 are typically pro-inflammatory, which means they can be activated during cell injury, infection, invasion, and inflammation. Some pro-inflammatory cytokines include:
- Interferon-γ
- Tumor necrosis factor-α
- Interleukin-1β (IL-1β)
- IL-6
On the other hand, cytokines produced by Th2 are anti-inflammatory and help control the Th1 cytokine response. Major anti-inflammatory cytokines include:
- IL-4
- IL-5
- IL-10
- IL-11
- IL-13
Your immune system needs a balance of Th1 and Th2 responses to prevent excess inflammation. Therefore, inflammation can be a result of a disruption in the Th1: Th2 balance.
Additionally, pro-inflammatory cytokines overstimulate the microglia, a group of specialized cells whose primary job is to clean out damaged neurons and maintain a healthy nervous system. Overstimulated microglia results in a significant increase in the production of pro-inflammatory cytokines, such as IL-1β, as well as neurotoxic substances like reactive oxygen species. Microglia are also the only type of cell in the central nervous system capable of producing quinolinic acid – a potent neurotoxin and contributor to depression.
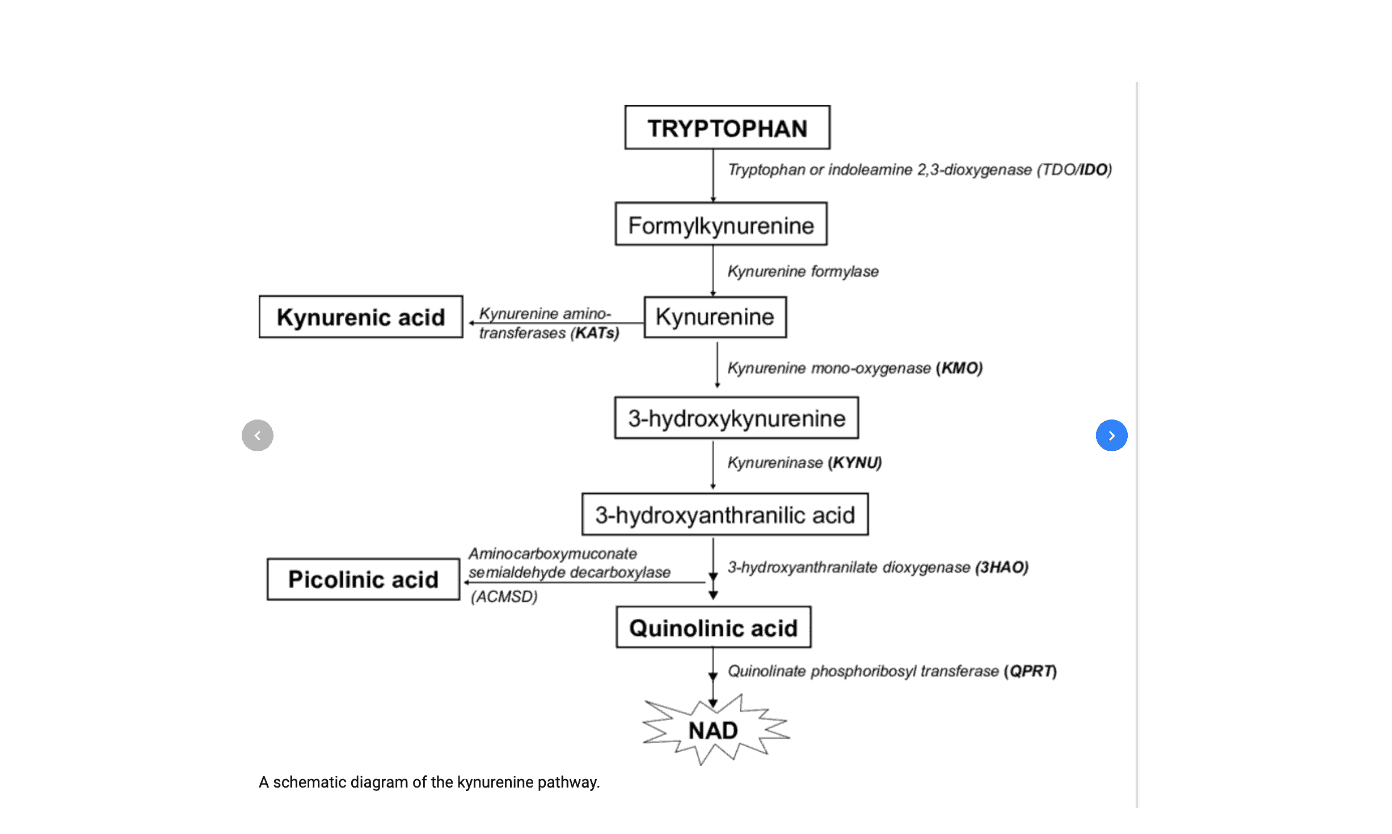
Essentially, these processes compound on one another ultimately leading to a cascade of factors all able to worsen depression. Up next is the tryptophan pathway, where a seemingly subtle shift from one end product to another can cause all sorts of problems – like a train that’s jumped tracks.
The Link Between Tryptophan and Depression
Inside the brain, pro-inflammatory cytokines significantly influence four important neurotransmitters:
- Serotonin: The “happy chemical.”
- Dopamine: Involved in body movement, memory, learning, attention, and motivation.
- Noradrenaline: Involved in the fight-or-flight response.
- Glutamate: The most abundant neurotransmitter in our brain.
Of the four neurotransmitters above, you’d probably guess that serotonin plays a role in depression. And you’d be correct! However, scientists are finding there’s more to it than we once thought.
What you may not know is that the precursor to serotonin is tryptophan, an essential amino acid important for normal neurobehavior. According to the “serotonin hypothesis,” depression can be caused by a shunt of tryptophan away from serotonin to kynurenine, depleting the tryptophan supply. Essentially, the theory states that when more tryptophan becomes kynurenine instead of serotonin than what’s typical, it can lead to depression.
However, the conversion of tryptophan to serotonin only happens in about 5% of tryptophan. The other 95% of tryptophan goes down the kynurenine pathway. In short, tryptophan gets converted into kynurenine, a contributor to anxiety. From there, kynurenine gets further degraded into different metabolites:
- Quinolinic acid
- Kynurenic acid
Both quinolinic acid and kynurenic acid are kynurenine metabolites that are involved in inflammation, nerve stimulation, and immune responses.
So in the case of depression, not only is less tryptophan becoming serotonin the “happy chemical” but it’s going down a path to become pro-inflammatory which further contributes to the condition.
You can read more about tryptophan's role in depression in my article: Tryptophan: Beyond Thanksgiving – It’s Role in Happiness, Depression, and Suicide
When Glutamate Goes From Excited to Hyper
The amino acid glutamate is very important to the central nervous system. Glutamate is the main excitatory neurotransmitter in your brain, which your nerve cells need for sending signals to one another. Glutamate is also involved in learning and memory. But glutamate can also be neurotoxic at excessive levels when receptors are overstimulated – like that sudden shift when a child goes from excited to hyper.
Let’s look at the mechanism behind inflammation and glutamate production.
One predominant receptor involved in depression is called N-methyl-D-aspartate (NMDA). As you read earlier, microglia produces the pro-inflammatory cytokine IL-1β. In turn, IL-1β increases the expression of the NMDA receptor. As we saw in the previous section, much of the tryptophan supply in our bodies gets converted into quinolinic acid and kynurenic acid, both of which bind to the NMDA receptor.
However, there’s more to this story. While they both bind to NMDA, kynurenic acid and quinolinic acid act differently – kynurenic acid blocks the receptor while quinolinic acid activates it. Pro-inflammatory cytokines, through the activation of microglia, cause a higher ratio of quinolinic acid to kynurenic acid, leading to overstimulation of the NMDA receptor.
The activation of the NMDA receptor doesn’t just release glutamate. It further activates microglia, which only releases pro-inflammatory cytokines. IL-1β also produces a toxic substance called nitric oxide, resulting in more glutamate – another cascading effect.
Fortunately, we have helpful star-shaped glial cells called astrocytes, which are responsible for taking up excess glutamate. Astrocytes help protect neurons from toxic effects. However, astrocytes can be the target of pro-inflammatory cytokines, which as we now know are running rampant in people with depression.
Although the exact mechanisms are still unclear, some scientists believe that inflammation leads to a decrease in astrocyte density. This disrupts neuroplasticity, the brain's ability to reorganize itself in response to injury and disease. To make things worse, once microglia are activated, they stay stimulated for several months, trapping your brain in a vicious inflammatory cycle.
This is yet another example of a runaway train effect that may make it harder for those with depression to heal. Though keep in mind, this was a deep dive into the emerging science behind depression so all hope isn’t lost!
In fact, I’d argue our better understanding of the mechanisms behind depression is giving us insight into more effective treatments. With better understanding comes an improved capacity to heal.
How Do You Begin to Heal?
The modern treatment models of depression are inadequate. And the numbers don’t lie – at least 50% of those who recover from their first episode of depression experience one or more additional episodes in their lifetime.
But there is some good news. Recent research shows that ketamine, an NMDA blocker, may be an effective treatment for depression.
If you are looking for a way to treat your depression without relying on antidepressants or anti-inflammatory agents, I’ve written several blog posts about drug-free depression treatment, including 6 simple steps you can take to start your journey today.
Are you surprised that inflammation plays such an important role in depression? Have you or a loved one experienced depression that didn’t get better with the traditional antidepressants? I’d love to hear from you.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4292164/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2785020/
https://www.bmj.com/content/321/7258/424.1
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4141874/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3021918/
https://pdfs.semanticscholar.org/6bac/723741ca2f7a77b9e631540a0d951ff3a931.pdf
https://www.ncbi.nlm.nih.gov/pubmed/10736372
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181613/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC443394/
https://www.ncbi.nlm.nih.gov/pubmed/9523571
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3799810/
https://www.ncbi.nlm.nih.gov/pubmed/11126389
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2169519/
https://ebmh.bmj.com/content/19/2/35
https://www.ncbi.nlm.nih.gov/pubmed/18567974
* These statements have not been evaluated by the Food and Drug Administration. The product mentioned in this article are not intended to diagnose, treat, cure, or prevent any disease. The information in this article is not intended to replace any recommendations or relationship with your physician. Please review references sited at end of article for scientific support of any claims made.













13 Comments
This isn’t obvious to a lot of people YET but all of the above are changes in the brain FROM guilt and other feelings being harbored, they are not causative of these feelings. When you change the feelings, you change the brain, and lose the disease. Analyzing all these effects from depression is just that. It’s not addressing the cause. When you stop beating yourself up and being perfectionistic and setting overly high expectations for yourself, the disease dissolves.
Thanks for the post. When I saw your mention of the “embodied cognition” concept, I was reminded of the brain circuit that has been hypothesized to be the anatomic correlate to the “ego” Michael Pollan, in his recent book “How to Change Your Mind”, addresses the “default mode network” which is comprised of the following anatomic structures in the brain:
medial prefrontal cortex
posterior cingulate cortex
inferior parietal lobule
lateral temporal cortex
dorsal medial prefrontal cortex
hippocampal formation
If this network is indeed the anatomic foundation of the ego, and if egocentricity is a key player in depression (which I believe it is), then addressing down-regulation of this circuit might have a tremendous impact on depression.
Hello Dr. Jill Carnahan, thank you so much for your blog which is invaluable to me!!! I am trying to apply the Bredesen protocol to my mother with early AD. We live in France and there is, unfortunately, no doctor trained in functional medicine here.
My mother has been taking 5HTP (50mg / 1 per day) for 3 months now. I understood from your article it is not so good to take tryptophan. Do you think my mother can stop this supplement overnight (with no specific risks)?
Would it be a good idea to stop it? (She is very anxious and depressive despite the fact she takes Rhodiola – bacopa – Gotu Kola and she follows all the recommendations listed in the “6 simple steps”).
(Unfortunately, I cannot rely on any French medical doctor in her town as they do not know anything about this and will immediately prescribe anti-depressants…)
Not everyone reacts to tryptophan or 5HTP but certain people do… she would feel more depression or anxiety if she is reacting to the 5HTP
Thank you very much! If my mother tries to stop 5HTP, do you think she can do it overnight (without any specific risks) ?
yes likely safe to stop
Hi Jill, Excellent overview! Thank you!
Thanks for info. The salmon oil you suggest comes in 500 mg. and 1000…which one should we take 3 of every day?
1000mg
Dr. Carnahan,
This is a well written article.
Since you are not accepting new patients at this time, do you have a list of providers that believe in / agree with you with the inflammation theory?
Would anyone else on your team be able to assist?
I have been suffering with anxiety and depression and would like to consult with someone who really understands brain inflammation and wants to help.
Regards,
Raj
Thank you, Rajan
I have a great article here on how to choose a good functional medicine trained physician
warmly
Dr Jill
I have read for years that there are many different inflammatory pathways. However; some research I’ve read indicates that all of these pathways (and the inflammatory response itself) may have a “master switch”, controlled by something called Nuclear factor κ B (NF-kB). And if drugs can be developed to control this one inflammatory pathway, inflammation throughout the entire body can (in theory) be regulated. Is there any truth to this inflammatory “master switch” theory regarding NF-kB?
Share: